Aging, Obesity & Muscle Loss: Can Exercise Reverse the Damage?
Discover the surprising link between **aging, obesity, and muscle decline**—and how **exercise** can help reverse the damage. Learn the latest research on **cellular senescence, insulin sensitivity, and muscle regeneration** to stay strong and healthy as you age.
DR T S DIDWAL MD
3/29/20259 min read

Exercise and Metabolic Health: Impact on Cellular Aging, Insulin Sensitivity, and Systemic Health
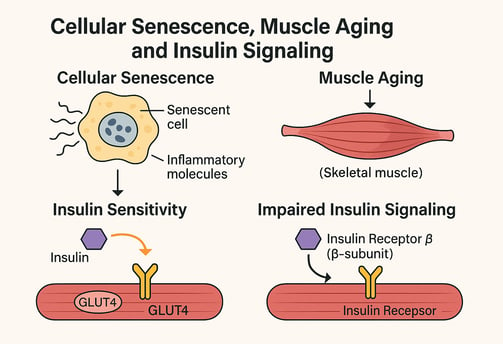
Did you know that cellular senescence (CS) plays a major role in aging, particularly in skeletal muscle (SkM)? As we age, senescent cells accumulate, leading to muscle loss (sarcopenia) and insulin resistance—especially in individuals with obesity. While exercise is widely recognized for boosting metabolic health and muscle function, its direct impact on CS has remained unclear.
This study explored the effects of exercise on CS by analyzing muscle biopsies from both young, normal-weight individuals and middle-aged individuals with obesity, before and after an exercise intervention. Researchers found that individuals with obesity had significantly higher CS markers, lower GLUT4 and PAX7 expression, and reduced insulin sensitivity. However, after exercise, these markers improved—showing enhanced insulin signaling and muscle regeneration.
In vitro experiments further revealed that senescence disrupts satellite cell function, a key player in muscle repair, by downregulating essential regulatory genes and impairing the Insulin Receptor β-subunit. These findings highlight the potential of exercise as a powerful tool to counteract CS, improve muscle health, and reduce age- and obesity-related dysfunction. Future therapies targeting senescent cells, either through exercise or senolytic agents, could revolutionize treatments for sarcopenia and metabolic disorders.
Cellular Senescence and Exercise: Fighting Aging at the Cellular Level
Understanding Cellular Senescence in Skeletal Muscle
Cellular senescence (CS) represents a critical aging process characterized by irreversible cell cycle arrest and an altered secretory phenotype. In skeletal muscle, the accumulation of senescent cells contributes significantly to sarcopenia – the age-related loss of muscle mass and function that affects quality of life and increases mortality risk in older adults.
Recent research examined muscle biopsies from two distinct groups: young, normal-weight individuals and middle-aged individuals with obesity. The study investigated how exercise interventions affected markers of cellular senescence in skeletal muscle tissue.
Key Findings on Exercise and Cellular Senescence
The research revealed that individuals with obesity displayed significantly elevated CS markers, alongside reduced expression of GLUT4 (a glucose transporter) and PAX7 (a satellite cell marker). These findings indicate impaired insulin action and diminished regenerative potential in the skeletal muscle of these individuals.
The exciting news? Exercise intervention reduced CS markers and activated satellite cell response in both groups, although the effect was more pronounced in younger participants. These improvements corresponded with enhanced insulin sensitivity, suggesting that exercise's metabolic benefits may be partially mediated through its ability to counteract cellular senescence.
In vitro experiments further demonstrated that senescence downregulates key regulatory genes in satellite cells and impairs insulin signaling by reducing the Insulin Receptor β-subunit. This provides a mechanistic explanation for how cellular senescence contributes to metabolic dysfunction in aging and obesity.
These findings highlight the therapeutic potential of exercise in mitigating age- and obesity-related muscle dysfunction, suggesting that targeting cellular senescence through exercise or senolytic agents could offer promising strategies for improving metabolic health and combating sarcopenia.
Exercise and Liver Health: The Neuregulin-4 Connection
The Role of Adipokines in Exercise-Induced Metabolic Improvements
Beyond its effects on skeletal muscle, exercise positively impacts liver health, particularly in conditions like metabolic dysfunction-associated steatotic liver disease (MASLD). One mechanism involves Neuregulin-4 (Nrg4), an adipokine that plays a potential role in metabolic homeostasis.
Uncovering the Nrg4 Mechanism
Research using mouse models has discovered that adipose Nrg4 is upregulated by exercise through activation of PPARγ. This exercise-induced increase in Nrg4 appears crucial for ameliorating liver steatosis, as demonstrated through several experimental approaches:
Adeno-associated virus (AAV)-mediated knockdown of adipose Nrg4 impaired exercise-mediated alleviation of MASLD
Hepatocyte-specific knockout of Erbb4 (the Nrg4 receptor) similarly reduced exercise benefits
Conversely, AAV-mediated overexpression of adipose Nrg4 mitigated MASLD in mice, working synergistically with exercise
The underlying mechanism involves Nrg4/Erbb4/AKT signaling, which promotes phosphorylation of cyclic guanosine monophosphate-AMP synthase (cGAS), blunting its enzyme activity and thereby inhibiting inflammation and steatosis in hepatocytes.
This research elegantly demonstrates how Nrg4 functions as an exercise-induced adipokine that facilitates adipose-liver tissue communication to counteract MASLD, highlighting the complex inter-organ crosstalk that mediates exercise's systemic benefits.
Epigenetic Modifications: How Exercise Rewrites Our Genetic Expression
Exercise-Induced Epigenetic Adaptations
The relationship between exercise and gene expression represents an exciting frontier in exercise physiology. Physical activity and exercise trigger adaptive responses in skeletal muscle through epigenetic modifications – changes that affect gene expression without altering the underlying DNA sequence.
Recent research has identified various epigenetic markers linked to physical activity and exercise, with the most critical being DNA methylation and histone modifications. These changes are associated with the transcriptional response of skeletal muscle to exercise and facilitate adaptation to training.
Other emerging epigenetic processes involved in exercise adaptation include:
Acetylation as a new epigenetic modification
Changes mediated by methylation and phosphorylation
Micro-RNA (miRNA) regulation
These epigenetic mechanisms help explain why both endurance training (ET) and resistance training (RT) can trigger distinct metabolic and structural adaptations in skeletal muscle, ultimately impacting health outcomes through altered gene expression patterns.
Women's Health: Exercise, Eating Behavior, and Cardiovascular Protection
Research Findings on Postmenopausal Women
A recent study from the University of Jyväskylä has revealed important insights into women's metabolic health, particularly after menopause. Researchers found that women exhibiting disturbed eating behaviors combined with low physical activity tend to accumulate more central body fat and show higher risk of metabolic low-grade inflammation – a condition that increases the risk of cardiovascular diseases.
This risk becomes particularly relevant after menopause, when cardiovascular disease prevalence rises significantly. However, the research offered a promising finding: the combined effect of exercise and healthy eating behavior provides the most effective protection against inflammation and may even reduce existing inflammation after menopause.
This study underscores the importance of addressing both physical activity levels and eating patterns as interconnected factors in women's cardiovascular health, especially during and after the menopausal transition.
Beyond Muscle: How Exercise Benefits Multiple Organ Systems
The Multi-Organ Effects of Exercise
While much research focuses on skeletal muscle adaptations to exercise, regular physical activity exerts profound metabolic benefits through multiple tissues, including:
Liver: Improved glucose metabolism and reduced fat accumulation
Adipose tissue: Enhanced insulin sensitivity and altered secretory profile
Vasculature: Improved endothelial function and reduced inflammation
Pancreas: Enhanced insulin production and secretion
A growing body of evidence suggests that exercise induces inter-tissue communication through various signaling molecules, hormones, and cytokines collectively termed "exerkines." These exercise-induced factors coordinate metabolic adaptations across different organs, contributing to exercise's robust protective effects against metabolic diseases like type 2 diabetes and non-alcoholic fatty liver disease.
This whole-body perspective helps explain why exercise is such a powerful protective agent against metabolic disease – it simultaneously improves metabolic function in multiple organs, creating synergistic health benefits that exceed what would be expected from any single tissue adaptation.
Maternal Exercise and Offspring Health: Intergenerational Benefits
Transgenerational Effects of Exercise
An intriguing area of research examines whether maternal exercise during pregnancy can improve the metabolic health of offspring. While research in this area continues to develop, emerging evidence suggests that maternal physical activity may program offspring metabolism in favorable ways, potentially reducing their future risk of metabolic disorders.
Potential mechanisms include:
Epigenetic modifications transmitted to offspring
Improved placental function and nutrient delivery
Reduced maternal inflammation and oxidative stress
Altered hormonal environment during critical developmental periods
This research highlights how the benefits of exercise may extend beyond the individual, potentially influencing metabolic health across generations and offering a compelling public health perspective on physical activity promotion.
FAQs About Exercise and Metabolic Health
How does exercise affect metabolism?
Exercise affects metabolism through both acute and chronic mechanisms. Acutely, each exercise session increases energy expenditure, improves glucose uptake in muscles, and enhances fat oxidation. Chronically, regular exercise increases mitochondrial density and function, improves insulin sensitivity, reduces inflammation, and creates favorable changes in body composition. These adaptations collectively enhance metabolic flexibility – the ability to efficiently switch between different fuel sources based on availability and demand.
How does physical activity affect skeletal muscle physiology?
Physical activity triggers numerous adaptations in skeletal muscle, including increased capillary density, enhanced mitochondrial function, improved calcium handling, and altered fiber type composition. These changes are orchestrated through complex signaling pathways activated by mechanical stress, metabolic demands, and hormonal factors during exercise. The type of exercise (endurance vs. resistance) determines the specific adaptations, with endurance training primarily enhancing oxidative capacity and resistance training promoting structural protein synthesis.
How does exercise affect myofiber metabolism?
Exercise profoundly alters myofiber metabolism through multiple mechanisms. It increases glucose transporter (GLUT4) translocation to the cell membrane, enhances insulin signaling, upregulates enzymes involved in both glycolytic and oxidative energy systems, and improves mitochondrial function. These changes optimize energy production and substrate utilization during both rest and physical activity.
How does exercise affect skeletal muscle function?
Exercise improves skeletal muscle function through several adaptations: increased strength and power output, enhanced endurance capacity, improved coordination and motor control, and better neuromuscular efficiency. These functional improvements result from both structural changes within the muscle and neural adaptations that optimize muscle recruitment and firing patterns.
Is exercise a subcategory of physical fitness?
Physical fitness represents a state or condition, while exercise refers to structured physical activity performed with the goal of maintaining or improving physical fitness. Therefore, exercise is better understood as a means to achieve physical fitness rather than a subcategory of it. Physical fitness encompasses multiple components including cardiovascular endurance, muscular strength, flexibility, body composition, and neuromuscular coordination.
Does maternal exercise improve the metabolic health of the offspring?
Emerging research suggests that maternal exercise during pregnancy may positively influence offspring metabolic health through several mechanisms, including epigenetic modifications, improved placental function, and a more favorable intrauterine environment. These effects may reduce offspring risk for conditions like obesity and insulin resistance later in life, although more research is needed to fully understand these transgenerational benefits.
Key Takeaways: The Science of Exercise and Metabolic Health
Cellular senescence reduction: Exercise reduces markers of cellular senescence in skeletal muscle, potentially mitigating age- and obesity-related muscle dysfunction.
Improved insulin sensitivity: Regular physical activity enhances insulin action through multiple mechanisms, benefiting glucose metabolism throughout the body.
Liver health promotion: Exercise triggers the release of beneficial adipokines like Neuregulin-4 that protect against fatty liver disease through complex signaling pathways.
Epigenetic reprogramming: Physical activity induces epigenetic modifications that alter gene expression in ways that promote metabolic health and adaptation.
Inflammation reduction: Regular exercise, especially when combined with healthy eating behaviors, reduces systemic low-grade inflammation associated with cardiovascular disease risk.
Multi-organ benefits: Exercise simultaneously improves metabolic function in multiple organs including muscle, liver, adipose tissue, and pancreas.
Inter-tissue communication: Exercise coordinates metabolic adaptations across different organs through "exerkines" that facilitate tissue crosstalk.
Potential transgenerational effects: Maternal exercise may program offspring metabolism in favorable ways, extending benefits across generations.
Conclusion: Exercise as Metabolic Medicine
The research summarized in this review paints a compelling picture of exercise as a powerful metabolic medicine with effects that extend from the cellular to the systemic level. By combating cellular senescence, enhancing insulin sensitivity, reducing inflammation, and orchestrating beneficial adaptations across multiple organ systems, physical activity offers a comprehensive approach to metabolic health that no pharmaceutical intervention can match.
What makes exercise particularly remarkable is its simultaneous impact on multiple physiological systems and its ability to be customized to individual needs, preferences, and limitations. Whether through endurance training, resistance exercise, or combined approaches, regular physical activity represents one of our most potent tools for preventing and managing metabolic disorders.
Call to Action: Translate Knowledge Into Movement
Understanding the science behind exercise's metabolic benefits provides powerful motivation for incorporating regular physical activity into daily life. Consider these steps to harness the metabolic power of movement:
Start where you are: Even modest increases in physical activity can trigger positive metabolic adaptations.
Embrace variety: Combine different exercise modalities to maximize diverse metabolic benefits.
Consistency over intensity: Regular, moderate exercise often yields greater long-term benefits than sporadic high-intensity workouts.
Personalize your approach: Consider your age, health status, preferences, and goals when designing your exercise routine.
Think beyond weight: Remember that many of exercise's most important metabolic benefits occur independently of changes in body weight or composition.
Partner with professionals: Work with healthcare providers, exercise physiologists, or certified fitness professionals to develop a safe, effective approach tailored to your needs.
By translating this scientific knowledge into consistent action, you can harness the remarkable power of exercise to optimize your metabolic health, prevent chronic disease, and enhance quality of life across the lifespan.
Related Article
Stronger Muscles, Sharper Mind: How Strength Training Boosts Brain Health
Live Longer, Stronger: The Ultimate Guide to Cardiorespiratory Fitness | Healthnewstrend
Does Muscle Loss Increase Dementia Risk? Scientists Say Yes | Healthnewstrend
Journal References
Podraza-Farhanieh, A., Spinelli, R., Zatterale, F., Nerstedt, A., Gogg, S., Blüher, M., & Smith, U. (2025). Physical training reduces cell senescence and associated insulin resistance in skeletal muscle. Molecular metabolism, 102130. Advance online publication. https://doi.org/10.1016/j.molmet.2025.102130
Chen, M., Li, Y., Zhu, J. Y., Mu, W. J., Luo, H. Y., Yan, L. J., Li, S., Li, R. Y., Yin, M. T., Li, X., Chen, H. M., & Guo, L. (2025). Exercise-induced adipokine Nrg4 alleviates MASLD by disrupting hepatic cGAS-STING signaling. Cell reports, 44(2), 115251. https://doi.org/10.1016/j.celrep.2025.115251
Mallett, G. The effect of exercise and physical activity on skeletal muscle epigenetics and metabolic adaptations. Eur J Appl Physiol 125, 611–627 (2025). https://doi.org/10.1007/s00421-025-05704-6
Lankila, H., Kekäläinen, T., Hietavala, E., & Laakkonen, E. K. (2025). A mediating role of visceral adipose tissue on the association of health behaviours and metabolic inflammation in menopause: a population-based cross-sectional study. Scientific Reports, 15(1). https://doi.org/10.1038/s41598-025-85134-8
Disclaimer
The information on this website is for informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition or treatment. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
About the Author:
Dr.T.S. Didwal, MD, is an experienced Internal Medicine Physician with over 30 years of practice. Specializing in internal medicine, he is dedicated to promoting wellness, preventive health, and fitness as core components of patient care. Dr. Didwal’s approach emphasizes the importance of proactive health management, encouraging patients to adopt healthy lifestyles, focus on fitness, and prioritize preventive measures. His expertise includes early detection and treatment of diseases, with a particular focus on preventing chronic conditions before they develop. Through personalized care, he helps patients understand the importance of regular health screenings, proper nutrition, exercise, and stress management in maintaining overall well-being.
