BCAA Catabolism: A Potential Key to Unlocking Improved Metabolic Health?
Elevated BCAA levels are linked to insulin resistance. Explore potential causes, research, and strategies to modulate BCAA catabolism and improve metabolic health.
DR T S DIDWAL MD
3/1/20246 min read
Branched-chain amino acids (BCAAs) are a group of three essential amino acids that make up about 35% of the protein in muscle tissue. They are called "branched chains" because their chemical structure is like a branch. BCAAs are broken down in the body for energy, and they can also be used to make new proteins.BCAAs have been shown to have several health benefits, including improving muscle growth and recovery, reducing fatigue, and boosting the immune system. They may also help to protect against some chronic diseases, such as heart disease, diabetes, and cancer. However, too much of a good thing can be bad. According to a new study published in the journal Nutrition & Diabetes, high levels of BCAAs in the blood have been linked to an increased risk of insulin resistance, a condition that can lead to type 2 diabetes. BCAAs may also contribute to other health problems, such as obesity, liver disease, and cognitive decline.
Key message
Dysfunctional BCAA catabolism has emerged as a potential factor in obesity and type 2 diabetes (T2D), and strategies to enhance it might be a novel treatment approach.
Background:
T2D is a major global health issue, often linked to obesity and reduced insulin sensitivity.
Recent evidence suggests that BCAA metabolism plays a key role in this process.
Elevated BCAA levels are consistently observed in individuals with obesity and T2D.
The underlying cause of these elevated levels and their link to insulin resistance remain unclear.
Potential mechanisms:
Dysfunctional BCAA catabolism in various tissues (muscle, liver and adipose) could contribute to BCAA accumulation.
Elevated BCAA levels might act as signaling molecules, disrupting insulin signaling pathways and leading to insulin resistance.
Evidence from research:
In vitro and animal studies suggest that manipulating the BCAA catabolism pathway affects glucose homeostasis and insulin sensitivity.
Studies in both rodents and humans, albeit limited in humans, provide proof-of-concept that enhancing BCAA catabolism improves glucose control in metabolic disorders.
Current and future perspectives:
This review discusses potential mechanisms linking BCAA catabolism and insulin resistance.
It also summarizes available tools to modulate BCAA catabolism in vivo, including pharmaceutical and lifestyle interventions.
The review proposes exploring strategies to increase BCAA catabolism or lower BCAA levels as a potential new treatment approach for obesity and T2D.
Remaining knowledge gaps:
Our understanding of tissue-specific BCAA catabolism in humans is still limited.
Further research is needed to fully understand the causal relationship between BCAA catabolism and insulin resistance.
Introduction
In the realm of metabolic health, insulin resistance stands as a formidable adversary, often associated with obesity and type 2 diabetes (T2D). Recent developments have shed light on a potential player in this intricate scenario: dysfunctional BCAA catabolism. Elevated levels of branched-chain amino acids (BCAA) in plasma have been consistently observed in individuals grappling with insulin resistance, but the exact nature of this connection remains elusive.
Delving into Potential Mechanisms
Dysfunctional BCAA Catabolism as a Culprit
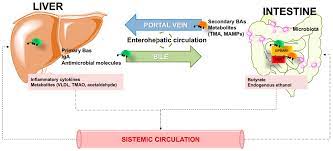
The roots of elevated BCAA levels may extend to dysfunctional catabolism in vital tissues such as muscle, liver, and adipose tissue. Disruptions in the breakdown pathway of BCAAs could contribute to their accumulation, creating a metabolic imbalance.
BCAA as Signaling Molecules
Furthermore, there's evidence suggesting that elevated BCAA levels might act as signaling molecules, meddling with insulin signaling pathways. This interference could potentially lead to insulin resistance, setting the stage for metabolic disorders.
Insights from Research
Both animal and human studies have embarked on the journey to unravel this intricate web. Manipulating the BCAA catabolism pathway appears to influence glucose homeostasis and insulin sensitivity. Proof-of-concept studies in rodents and humans showcase that enhancing BCAA catabolism holds promise for improving glucose control in metabolic disorders.
Current and Future Perspectives
Tools to Modulate BCAA Catabolism
In the pursuit of novel treatment approaches, researchers are exploring various tools to modulate BCAA catabolism in vivo. This includes both pharmaceutical and lifestyle interventions.
Strategies for the Future
This review goes beyond merely highlighting the issue. It proposes strategies to increase BCAA catabolism or lower BCAA levels as potential avenues for addressing obesity and T2D. However, our understanding of tissue-specific BCAA catabolism in humans is still in its infancy, prompting the need for further research.
Bridging Knowledge Gaps
Reduced BCAA Catabolism in Insulin Resistance
Examining plasma BCAA levels and insulin resistance reveals potential explanations. Reduced BCAA catabolism, attributed to decreased activity of key enzymes like BCAT and BCKD, emerges as a noteworthy factor. Lower expression of these enzymes in the tissues of individuals with insulin resistance and T2D underscores a potential link.
Altered BCAA Metabolism
Another facet of the puzzle involves altered BCAA metabolism, where these amino acids may be utilized less efficiently for energy production in insulin-resistant individuals, contributing to their accumulation in plasma.
Potential Mechanisms:
Several potential mechanisms have been proposed to explain how elevated BCAA levels may contribute to metabolic dysfunction. These mechanisms include:
Impaired insulin signaling: BCAAs may impair insulin signaling by activating the mTORC1 pathway, which regulates protein synthesis and cell growth.
Increased inflammatory response: BCAAs may promote inflammation by activating the NF-κB pathway, which is involved in the production of pro-inflammatory cytokines.
Enhanced lipogenesis: BCAAs may stimulate lipogenesis, the process of fat synthesis, by activating the SREBP-1c pathway, which is a key regulator of fatty acid synthesis.
Reduced mitochondrial function: BCAAs may impair mitochondrial function by inhibiting the activity of SIRT1, a protein that protects against mitochondrial dysfunction.
Unveiling Strategies to Lower BCAA Levels
Pharmaceutical Strategies:
GLP-1/GIP/Glucagon Receptor Agonists: Drugs like Tirzepatide, targeting these receptors, have shown promise in lowering blood sugar (glycemia) in type 2 diabetes (T2D) patients. Interestingly, these drugs also decrease BCAA and related metabolites in both mice and humans, potentially through altered gene expression regulating BCAA breakdown.
Glucagon Receptor Antagonists: These drugs improve insulin sensitivity in animal models of diabetes and obesity. Studies suggest they might work by enhancing BCAA breakdown in the heart, leading to better insulin response and heart function.
Alternative Strategies:
Physical Activity and Exercise: While traditionally seen as having minimal impact on energy from amino acids, recent research suggests exercise, particularly endurance training, may increase BCAA breakdown. This is supported by lower BCAA levels observed in more active individuals and studies showing increased BCAA breakdown enzymes following exercise. However, the exact mechanisms and effects on metabolic health remain unclear, with some studies showing conflicting results.
Dietary BCAA Restriction: Limiting dietary BCAA intake has been shown to improve metabolic health in obese rodents, including reducing body fat and improving insulin sensitivity. These effects seem independent of changes in BCAA breakdown enzymes, suggesting the reduced BCAA levels themselves improve glucose uptake. Human studies are limited due to challenges with controlling other dietary factors. However, some studies show promising results, with short-term BCAA restriction in T2D patients leading to lower BCAA levels, improved insulin sensitivity, and changes in gut microbiome composition. Further long-term studies are needed to assess safety and effectiveness in humans with obesity and insulin resistance.
Cold Acclimatization: Exposing rodents to cold temperatures significantly reduces BCAA levels, likely due to increased uptake and burning of BCAA in brown adipose tissue (BAT), which generates heat. This suggests BCAA might be a crucial energy source for BAT during cold exposure. Interestingly, humans with higher BAT activity showed greater BCAA level reduction upon cold exposure, suggesting a potential link between BAT and BCAA metabolism. However, the exact relationship with thermogenesis (heat generation) needs further investigation.
Limitations and Conclusions:
While several strategies can modulate BCAA catabolism and levels, their mechanisms in humans are not fully understood. More research is needed to optimize these strategies and determine if changes in BCAA catabolism directly contribute to improved metabolic health. Notably, only two interventions, BT2 and NaPB, directly target the BCAA breakdown pathway to improve glucose control. Other strategies, including those that improve overall metabolic health, have been shown to influence BCAA catabolism, but whether this is the mechanism behind their beneficial effects requires further investigation.that
Key Points
Insulin Resistance Challenge: Addressing the major health issue of insulin resistance linked to obesity and type 2 diabetes.
BCAA's Role: Unveiling the consistent elevation of plasma BCAA levels in individuals with insulin resistance, raising questions about its connection.
Potential Mechanisms: Exploring dysfunctional BCAA catabolism as a contributor and elevated BCAA levels as potential disruptors in insulin signaling pathways.
Research Insights: summarizing findings from animal and human studies that highlight the impact of manipulating the BCAA catabolism pathway on glucose control.
Current and Future Perspectives: Discussing strategies to modulate BCAA catabolism, including pharmaceutical and lifestyle interventions, as potential treatments for obesity and T2D.
Knowledge Gaps: Recognizing the need for further research, particularly in understanding tissue-specific BCAA catabolism in humans and the causal relationship with insulin resistance.
Practical Strategies: Exploring pharmaceutical interventions like BT2 and NaPB, alongside alternative approaches such as physical activity and dietary restrictions, as potential avenues for improving metabolic health.
Conclusion
In navigating the complex landscape of insulin resistance and metabolic disorders, understanding the nuances of BCAA catabolism becomes paramount. This article has unraveled the intricate web connecting dysfunctional BCAA catabolism to insulin resistance, offering insights into potential strategies and interventions. As we journey towards enhanced metabolic health, continued research will undoubtedly pave the way for innovative treatments.
References
Vanweert, F., Schrauwen, P., & Phielix, E. (2022). Role of branched-chain amino acid metabolism in the pathogenesis of obesity and type 2 diabetes-related metabolic disturbances BCAA metabolism in type 2 diabetes. Nutrition & Diabetes, 12(1), 1–13. https://doi.org/10.1038/s41387-022-00213-3
Related
https://healthnewstrend.com/polycystic-ovary-syndrome-and-type-2-diabetes-whats-the-link
https://healthnewstrend.com/ketogenic-diets-and-insulin-sensitivity-beyond-weight-loss
https://healthnewstrend.com/conquering-type-2-diabetes-with-exercise-a-guide-to-the-best-workouts
Medical Disclaimer
The information on this website is for informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition or treatment. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
