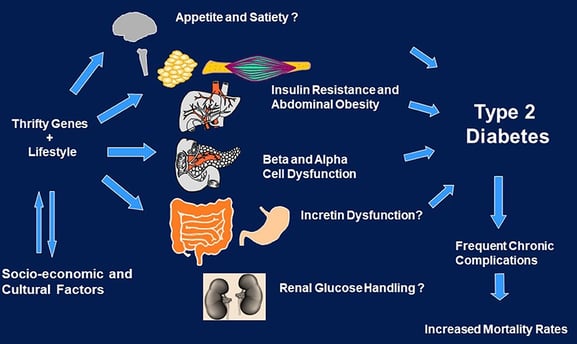
Diabetes Prevention: Multiple Metabolic Factors Fuel Diabetes
Discover how multiple metabolic factors, including BMI, BRI, pulse pressure, triglycerides, and HDL cholesterol, can significantly increase your risk of developing type 2 diabetes. Learn about the importance of addressing these factors for effective diabetes prevention
DR T S DIDWAL MD (Internal Medicine)
10/24/20248 min read
The study published in Nutrition and Metabolism revealed that multiple metabolic abnormalities, including body mass index (BMI), body roundness index (BRI), pulse pressure (PP), triglycerides (TG), and high-density lipoprotein (HDL) cholesterol, increase the risk of developing Type 2 diabetes. The more metabolic factors that were elevated over time, the higher the risk of diabetes. This research highlights the importance of a comprehensive approach to metabolic health, including regular monitoring of all metabolic parameters, early intervention, and addressing multiple risk factors simultaneously.
Key points
Multiple metabolic factors, including BMI, BRI, PP, TG, and HDL cholesterol, can increase the risk of Type 2 diabetes.
The more elevated metabolic factors over time, the higher the risk of diabetes.
Regular monitoring of all metabolic parameters is crucial for diabetes prevention.
Addressing metabolic abnormalities early, even before blood sugar levels become elevated, is critical.
Healthcare providers should consider the cumulative effect of multiple metabolic parameters when assessing diabetes risk.
A holistic approach to metabolic health, including lifestyle modifications that impact multiple parameters, is important for diabetes prevention.
The Perfect Storm: How Multiple Metabolic Factors Combine to Increase Diabetes Risk
Recent research has unveiled crucial insights into how various metabolic factors work together to increase the risk of Type 2 diabetes (T2D). A comprehensive study of over 78,000 adults in China has revealed that when multiple metabolic abnormalities persist over time, they create a compounding effect that significantly elevates diabetes risk. Let's dive into what this means for public health and personal wellness.
The Growing Diabetes Crisis
Type 2 diabetes has become a global health emergency. According to the International Diabetes Federation, the number of people living with diabetes is expected to reach a staggering 783 million by 2045, affecting 12.2% of the global population. This isn't just a statistic; it represents millions of lives impacted by a condition that can lead to serious health complications.
The Study: A Closer Look at Metabolic Risk Factors
This groundbreaking research examined how five key metabolic parameters interact over time to influence diabetes risk:
Body Mass Index (BMI)
Body Roundness Index (BRI)
Pulse Pressure (PP)
Triglycerides (TG)
High-Density Lipoprotein (HDL) cholesterol
The Snowball Effect
The study's findings were striking: the more metabolic factors that were elevated over time, the higher the risk of developing Type 2 diabetes. Specifically:
People with 1-2 elevated parameters had a 41% higher risk
Those with 3 elevated parameters saw their risk nearly double
Individuals with 4-5 elevated parameters had a 121% higher risk
Understanding Each Risk Factor
Body Measurements: BMI and BRI
Both BMI and BRI emerged as crucial indicators of diabetes risk. While BMI has long been recognized as a risk factor, BRI is a newer measure that combines height, waistline, and weight to better reflect visceral fat distribution. The mechanism behind this connection involves:
Insulin resistance
β-cell dysfunction
Chronic inflammation
The study confirms that maintaining a healthy weight isn't just about appearance; it's about preventing a cascade of metabolic disruptions that can lead to diabetes.
Blood Pressure: The Pulse Pressure Connection
One of the study's most interesting findings involves pulse pressure, which is the difference between systolic and diastolic blood pressure A normal pulse pressure for a healthy adult is between 40 and 60 millimeters of mercury (mmHg). A pulse pressure reading below 40 mmHg is considered low, and a reading above 60 mmHg is a risk factor for heart disease High pulse pressure over time increases diabetes risk through:
Endothelial dysfunction
Impaired insulin delivery to muscles
Reduced glucose uptake
This highlights the importance of maintaining healthy blood pressure, even if you're not currently at risk for diabetes.
Blood Lipids: The TG-HDL Dynamic
The relationship between triglycerides and HDL cholesterol reveals a complex interplay in diabetes risk:
1. High triglycerides can:
Contribute to insulin resistance
Impair insulin signaling
Worsen glucose intolerance
2. Low HDL levels are problematic because HDL:
Helps maintain pancreatic β-cell function
Enhances insulin sensitivity
Contains protective components like apolipoprotein A-I
The Fasting Glucose Factor
Perhaps most concerning is how these risks multiply when combined with elevated fasting plasma glucose (FPG), even within the normal range. The study found that individuals with:
The highest quartile of FPG
Plus 4-5 elevated metabolic parameters
Had a shocking 14.6 times higher risk of developing Type 2 diabetes compared to those with low FPG and no elevated parameters.
Key mechanisms for each metabolic factor:
1. Obesity (High BMI/BRI) mechanisms:
Adipose tissue dysfunction: Excess fat tissue releases inflammatory cytokines (like TNF-α and IL-6) that interfere with insulin signaling
Free fatty acid overflow: Excess fat releases too many free fatty acids, which:
Accumulate in liver and muscle, causing insulin resistance
Impair insulin secretion from pancreatic β-cells
Trigger chronic inflammation
Endocrine effects: Fat tissue produces hormones (adipokines) that affect metabolism.
Decreased adiponectin (which normally improves insulin sensitivity)
Increased resistin (which promotes insulin resistance)
2. High Pulse Pressure mechanisms:
Endothelial dysfunction: High PP damages blood vessel lining, leading to:
Reduced nitric oxide production (important for insulin action)
Impaired insulin delivery to muscles
Microvascular damage: affects small blood vessels that:
Reduces glucose uptake by muscles
Impairs insulin transport across vessel walls
Inflammation: Vessel damage triggers inflammatory responses that contribute to insulin resistance
3. Triglycerides (TG) mechanisms:
Direct cellular effects:
TGs accumulate in muscle and liver cells
This interferes with insulin signaling pathways
Causes "lipotoxicity" in pancreatic β-cells
VLDL overproduction:
High TGs lead to increased VLDL production in liver
This creates a cycle of worsening insulin resistance
Inflammatory effects:
High TGs promote inflammation
This further impairs insulin sensitivity
4. Low HDL mechanisms:
Reduced β-cell protection:
HDL normally protects insulin-producing cells
Low HDL means less protection from oxidative stress
Results in impaired insulin production
Decreased insulin sensitivity:
HDL components like apolipoprotein A-I enhance insulin sensitivity
Low HDL means reduced insulin-sensitizing effects
Anti-inflammatory properties lost:
HDL normally has anti-inflammatory effects
Low HDL allows more inflammation, promoting insulin resistance
5. Synergistic Effects:
Vicious cycle: Each factor can worsen the others
Inflammatory amplification: Multiple factors trigger more inflammation than any single factor
Oxidative stress: Combined effects create more oxidative damage
Mitochondrial dysfunction: Multiple factors impair cellular energy production
Endoplasmic reticulum stress: Combined metabolic stress affects protein folding and cellular function
Implications for Prevention
This research has significant implications for how we approach diabetes prevention:
1. Comprehensive Monitoring
Regular monitoring of all metabolic parameters is crucial, especially for:
Adults over 45
People with a family history of diabetes
Individuals with prediabetes
2. Early Intervention
The study suggests that addressing metabolic abnormalities early is critical, even before blood sugar levels become elevated. This might include:
Regular physical activity
Dietary modifications
Stress management
Regular health screenings
3. Risk Stratification
Healthcare providers should consider the cumulative effect of multiple metabolic parameters when assessing diabetes risk, rather than focusing on individual factors in isolation.
The Prediabetes Connection
The study also examined how these metabolic factors affect prediabetes progression and regression. This is crucial because:
5-10% of people with prediabetes develop T2D annually
Proper intervention can help reverse prediabetes
Multiple metabolic abnormalities make prediabetes more likely to progress to diabetes
Practical Takeaways
For individuals concerned about diabetes risk, this research suggests several key actions:
1. Regular Monitoring
Track all metabolic parameters, not just blood sugar
Pay attention to trends over time
Don't ignore "borderline" elevated results
2. Comprehensive Approach
Address all aspects of metabolic health
Work with healthcare providers to develop personalized strategies
Consider lifestyle modifications that impact multiple parameters
3. Early Action
Don't wait for prediabetes to make changes
Address elevated parameters even if blood sugar is normal
Focus on prevention rather than treatment
Looking Forward
This research opens new avenues for diabetes prevention and highlights the importance of a holistic approach to metabolic health. The findings suggest that:
Prevention strategies should target multiple metabolic parameters
Long-term monitoring is crucial
Early intervention can significantly reduce risk
Conclusion
The study provides compelling evidence that the path to Type 2 diabetes is paved with multiple metabolic abnormalities working in concert. Understanding this interaction helps us better appreciate why comprehensive lifestyle modifications are so important in diabetes prevention.
For healthcare providers, this research emphasizes the need for regular monitoring of multiple metabolic parameters and early intervention when abnormalities are detected. For individuals, it highlights the importance of maintaining overall metabolic health, not just managing blood sugar levels.
The key message is clear: when it comes to preventing Type 2 diabetes, we need to look at the bigger picture of metabolic health. By understanding and addressing multiple risk factors early, we can significantly reduce the risk of developing this serious chronic condition.
Remember: While this research provides valuable insights, always consult with healthcare professionals for personalized medical advice and treatment plans. They can help interpret your individual risk factors and develop appropriate prevention strategies based on your specific situation.
FAQs
1. What is the significance of this study?
This study provides crucial insights into how various metabolic factors work together to increase the risk of Type 2 diabetes. It highlights the importance of a comprehensive approach to metabolic health, emphasizing the need to address multiple risk factors simultaneously.
2. What are the key metabolic factors identified in the study?
The study focused on five key metabolic parameters: body mass index (BMI), body roundness index (BRI), pulse pressure (PP), triglycerides (TG), and high-density lipoprotein (HDL) cholesterol.
3. How does the combination of these factors affect diabetes risk?
The study found that the more metabolic factors that were elevated over time, the higher the risk of developing Type 2 diabetes. Individuals with multiple elevated parameters had a significantly increased risk compared to those with fewer abnormalities.
4. What are the implications for diabetes prevention?
The research suggests that regular monitoring of all metabolic parameters, early intervention when abnormalities are detected, and addressing multiple risk factors simultaneously are crucial for diabetes prevention.
5. Can this study help individuals assess their personal risk?
Yes, this study can help individuals understand the factors that contribute to their diabetes risk. By monitoring their own metabolic parameters and consulting with healthcare professionals, they can take proactive steps to reduce their risk.
6. Are there specific lifestyle changes that can address these metabolic factors?
Yes, lifestyle modifications such as regular physical activity, a healthy diet, stress management, and maintaining a healthy weight can help improve metabolic health and reduce the risk of diabetes.
7. Should individuals with prediabetes be particularly concerned?
Yes, the study found that individuals with prediabetes who also have multiple elevated metabolic parameters are at a significantly increased risk of developing Type 2 diabetes. Early intervention is crucial for these individuals.
8. Is this study applicable to all populations?
While the study was conducted in a Chinese population, the findings are likely applicable to diverse populations as the metabolic factors identified are common risk factors for diabetes worldwide.
9. Are there any limitations to the study?
The study was observational, meaning it cannot definitively prove causation. However, the strong association between multiple metabolic factors and diabetes risk provides compelling evidence for the importance of addressing these factors.
10. What are the next steps in this area of research?
Further research is needed to explore the specific mechanisms by which these metabolic factors interact to increase diabetes risk. Additionally, studies investigating the effectiveness of different prevention strategies targeting multiple metabolic parameters are warranted.
Related Articles
1. Boost Your Metabolic Health : How Low-Fat Diets and Muscle Mass Can Help
2. Not All Fat Is Created Equal: How Body Fat Distribution Impacts Your Metabolic Health
3. Best Exercises for People with Diabetes: Benefits, Challenges, and Strategies
Journal Reference
Xiong, WY., Liu, YH., Fan, YB. et al. The joint effect of cumulative metabolic parameters on the risk of type 2 diabetes: a population-based cohort study. Nutr Metab (Lond) 21, 78 (2024). https://doi.org/10.1186/s12986-024-00848-2
Image credit: https://www.frontiersin.org/files/Articles/366279/fendo-09-00479-HTML/image_m/fendo-09-00479-g001.jpg
Disclaimer
The information on this website is for informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition or treatment. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
About the Author:
Dr.T.S. Didwal, MD, is an experienced Internal Medicine Physician with over 30 years of practice. Specializing in internal medicine, he is dedicated to promoting wellness, preventive health, and fitness as core components of patient care. Dr. Didwal’s approach emphasizes the importance of proactive health management, encouraging patients to adopt healthy lifestyles, focus on fitness, and prioritize preventive measures. His expertise includes early detection and treatment of diseases, with a particular focus on preventing chronic conditions before they develop. Through personalized care, he helps patients understand the importance of regular health screenings, proper nutrition, exercise, and stress management in maintaining overall well-being.
With a commitment to improving patient outcomes, Dr. Didwal integrates the latest medical advancements with a compassionate approach. He believes in empowering patients to take control of their health and make informed decisions that support long-term wellness.
