From NAFLD to MASLD: A New Era in Fatty Liver Disease Diagnosis and Treatment
Fatty liver disease is now called MASLD—Metabolic dysfunction-associated steatotic liver disease. Learn why the name changed, what it means for your health, and how it impacts diagnosis and treatment.
DR T S DIDWAL MD
4/10/20258 min read
From NAFLD to MASLD: Understanding the Evolution in Fatty Liver Disease Nomenclature
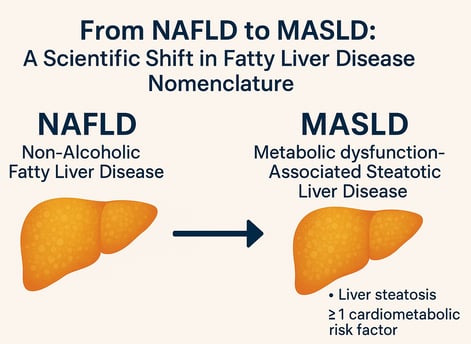
The recent transition from NAFLD (non-alcoholic fatty liver disease) to MASLD (metabolic dysfunction-associated steatotic liver disease) marks a pivotal shift in liver disease terminology. This change, adopted in 2023, highlights the central role of metabolic dysfunction—rather than alcohol exclusion—in driving liver fat accumulation. MASLD diagnosis now requires evidence of liver steatosis plus at least one cardiometabolic risk factor, offering greater diagnostic precision and improved risk stratification.
Importantly, the FDA approval of resmetirom in 2024 offers new hope for patients with MASH and fibrosis. Meanwhile, research into post-translational modifications (PTMs) is uncovering novel therapeutic targets. Though nearly all NAFLD patients meet MASLD criteria, this terminology update improves clinical clarity and supports global standardization in research and care.
As the burden of MASLD continues to grow, early screening, lifestyle intervention, and ongoing educational efforts will be key to reversing its trajectory and improving patient outcomes.
What Is MASLD?
Fatty liver disease affects over one-third of adults worldwide, and in 2023, doctors and scientists updated its name to better reflect what causes it. The old term—NAFLD (non-alcoholic fatty liver disease)—focused mostly on what didn't cause it (alcohol). The new name is MASLD, which stands for Metabolic dysfunction-Associated Steatotic Liver Disease.
Why the change? Because scientists now know that liver fat buildup is mainly caused by metabolic issues like obesity, type 2 diabetes, high blood pressure, and high cholesterol—not just alcohol. MASLD is diagnosed when there’s fat in the liver (seen through imaging or biopsy) and at least one metabolic risk factor.
MASLD includes a range of disease stages, from simple fat buildup to more serious problems like MASH (a form of liver inflammation), liver scarring (fibrosis), and even liver cancer. The good news? In early stages, MASLD can often be reversed with lifestyle changes like diet, exercise, and weight loss.
If you have conditions like obesity, diabetes, or metabolic syndrome, it’s a good idea to get your liver checked. MASLD can often be silent but may lead to serious complications if left untreated. Talk to your doctor about screening, prevention, and how to take care of your liver.
Under the updated diagnostic criteria, MASLD is diagnosed through a combination of:
MASLD (Metabolic dysfunction-Associated Steatotic Liver Disease): Requires evidence of liver steatosis (by imaging or biopsy) AND at least one of the following cardiometabolic risk factors:
Overweight/obesity
Type 2 diabetes
High blood pressure (hypertension)
Dyslipidemia (abnormal blood lipid levels)
Insulin resistance
MetALD (Metabolic dysfunction and Alcohol-associated Liver Disease): Requires evidence of liver steatosis, criteria for MASLD, AND significant alcohol consumption (typically >140g/week for women and >210g/week for men). This category identifies individuals with fatty liver due to a combination of metabolic dysfunction and alcohol intake.
Key Distinction: MASLD focuses on metabolic dysfunction as the primary driver, while MetALD acknowledges the combined impact of metabolic issues and alcohol. Other classifications exist for specific etiologies of liver disease.
Evidence of liver steatosis
Presence of at least one of five cardiometabolic risk factors
This shift addresses several limitations of the previous NAFLD terminology, which was defined primarily by exclusion (the absence of significant alcohol consumption) rather than by the actual mechanisms driving the disease.
The Spectrum of MASLD
MASLD encompasses a broad disease spectrum, ranging from:
Simple fatty liver (isolated hepatic steatosis)
Metabolic dysfunction-associated steatohepatitis (MASH) - the progressive inflammatory form
Advanced stages including fibrosis, cirrhosis, and hepatocellular carcinoma
This comprehensive umbrella term better reflects the progressive nature of the condition and its various manifestations. Importantly, MASH represents an active stage requiring pharmacological intervention, particularly when there is evidence of necroptotic damage with fibrotic progression.
The Global Burden of MASLD
MASLD affects more than one-third of adults worldwide, making it the most common chronic liver disease globally. This prevalence continues to rise alongside increasing rates of:
Obesity
Type 2 diabetes
Insulin resistance
Gut microbial dysbiosis
These interrelated conditions create a complex web of metabolic dysfunction that contributes to liver disease progression. The global burden of MASLD represents a major public health challenge, with significant implications for healthcare systems worldwide.
How Is MASLD Diagnosed Without a Biopsy?
Doctors can often check for MASLD using non-invasive tools, which means no needles or surgery. These tests are safe, quick, and painless:
FibroScan (Transient Elastography): A special ultrasound that measures liver stiffness and fat content.
ELF Test (Enhanced Liver Fibrosis): A blood test that checks for markers of liver scarring.
FIB-4 Index: A formula using simple blood tests (like liver enzymes, age, and platelet count) to estimate liver damage.
MRI-PDFF or Controlled Attenuation Parameter (CAP): Advanced imaging tools that assess how much fat is in the liver.
Key Advantages of the New MASLD Terminology
Enhanced Precision and Risk Stratification
The MASLD terminology offers greater precision in identifying at-risk individuals. By centering metabolic dysfunction as the primary criterion, clinicians can better stratify patients according to their risk profiles and tailor interventions more effectively.
Inclusion of Diverse Metabolic Profiles
The new nomenclature broadens the scope of liver disease classification by incorporating individuals with diverse metabolic profiles. This includes lean patients with hepatic steatosis who might have been overlooked under the previous NAFLD definition.
Alignment with Multifactorial Nature
MASLD better aligns clinical practice with the multifactorial nature of steatotic liver disease. It acknowledges the complex interplay of genetic, environmental, and metabolic factors that contribute to disease development and progression.
Standardization of Research and Clinical Practice
The global adoption of MASLD creates opportunities for standardization in both clinical and research settings. This facilitates:
Multicenter collaborations
Enhanced development of diagnostic tools
More targeted therapeutic strategies
Recent Research Insights on MASLD
Comparing NAFLD and MASLD Outcomes
Several recent studies have compared NAFLD and MASLD regarding mortality, liver-related outcomes, and extrahepatic events. Key findings include:
Most patients with NAFLD (approximately 99% in some studies) also meet the criteria for MASLD
Similar clinical profiles between the two diagnostic categories
No significant differences in mortality, liver-related outcomes, or extrahepatic events between NAFLD and MASLD cohorts
A Japanese study, for example, found a 99.3% overlap between patients diagnosed with NAFLD and those meeting MASLD criteria, with nearly identical clinical and biochemical profiles.
Latest Treatment Options for MASLD/MASH
Current FDA-Approved Treatment
Resmetirom (2024): First FDA-approved medication specifically for non-cirrhotic MASH with moderate to advanced fibrosis. Acts as a thyroid hormone receptor-β agonist that improves liver metabolism.
Emerging Pharmacological Approaches
GLP-1 Receptor Agonists: Semaglutide and tirzepatide show promising results in reducing liver fat and inflammation through weight loss and direct metabolic effects.
FXR Agonists: Obeticholic acid and other FXR agonists target bile acid pathways to reduce inflammation and fibrosis.
Combination Therapies: Dual and triple combination approaches targeting multiple pathways simultaneously show enhanced efficacy in clinical trials.
PPAR Agonists: Lanifibranor and other PPAR agonists demonstrate anti-inflammatory and anti-fibrotic effects.
Non-Pharmacological Interventions
Lifestyle Modification: Weight loss of 7-10% remains the most effective intervention for early-stage disease.
Bariatric Surgery: Shows significant improvement in MASH resolution and fibrosis regression in appropriate candidates.
Mediterranean Diet: Evidence supports its effectiveness in reducing liver fat independent of weight loss.
Pipeline Treatments in Late-Stage Development
Several promising candidates are in Phase III trials with potential approvals expected within the next 1-2 years, including novel anti-fibrotics and metabolic modulators.
The Role of Post-Translational Modifications (PTMs)
Emerging research highlights the importance of post-translational modifications (PTMs) in MASLD pathogenesis. These modifications influence:
Lipid metabolism
Inflammatory processes
Fibrosis development
Key PTMs implicated in MASLD include phosphorylation, ubiquitylation, acetylation, and glycosylation of proteins involved in liver metabolism. Understanding these modifications offers potential targets for novel therapeutic approaches.
Impact on Quality of Life
Studies using the Chronic Liver Disease Questionnaire (CLDQ)-NAFLD/NASH assessment tool have demonstrated that MASLD is associated with impaired patient-reported outcomes, including health-related quality of life. This highlights the importance of considering patient experience alongside clinical markers when evaluating disease impact and treatment effectiveness.
Challenges in MASLD Implementation
Despite its advantages, the transition to MASLD terminology faces several challenges:
Potential Confusion During Implementation
The shift from a well-established term (NAFLD) to a new designation (MASLD) may create temporary confusion among healthcare providers and patients during the transition period.
Cultural and Linguistic Barriers
Global adoption of MASLD requires overcoming cultural and linguistic barriers, ensuring consistent understanding and application across diverse healthcare systems.
Integration with Existing Nomenclature
The integration of related classifications, such as Metabolic dysfunction-Associated Liver Disease (MetALD), requires careful coordination to avoid diagnostic ambiguity.
Educational Needs
Comprehensive educational initiatives are needed for both healthcare providers and patients to ensure proper understanding and application of the new terminology and diagnostic criteria.
Targeting Metabolic Risk Factors
Comprehensive approaches to MASLD management must include addressing underlying metabolic risk factors, particularly obesity and type 2 diabetes, which drive disease progression.
Key Takeaways
MASLD represents an evolution in terminology that better reflects the metabolic underpinnings of fatty liver disease.
The new nomenclature improves risk stratification by incorporating metabolic criteria into the diagnostic process.
MASLD affects over one-third of adults worldwide, making it a significant public health concern.
The disease spectrum ranges from simple steatosis to cirrhosis and cancer, with MASH representing an active stage requiring intervention.
Recent approval of resmetirom marks a milestone in treatment options, though more therapeutic approaches are needed.
Post-translational modifications offer promising targets for future therapeutic development.
Educational initiatives are crucial for successful implementation of the new terminology.
Nearly all patients with NAFLD also meet MASLD criteria, suggesting high diagnostic overlap between the classifications.
Frequently Asked Questions
What is the main difference between NAFLD and MASLD?
While NAFLD was defined primarily by excluding significant alcohol consumption, MASLD is diagnosed through positive criteria: the presence of liver steatosis plus at least one metabolic risk factor. This shift emphasizes the metabolic dysfunction underlying the disease rather than defining it by what it is not.
Does the change from NAFLD to MASLD affect patient care?
The diagnostic criteria for MASLD may identify some patients who were previously missed under NAFLD definitions, particularly lean individuals with metabolic dysfunction. However, studies show substantial overlap between the two classifications, suggesting that most patients diagnosed with NAFLD would also meet MASLD criteria.
What treatments are available for MASLD?
Management strategies include lifestyle modifications (diet, exercise, weight loss), addressing underlying metabolic conditions, and in certain cases, pharmacological interventions. Resmetirom was recently approved specifically for MASH with fibrosis, and numerous other treatments are in development.
How is MASLD diagnosed?
Diagnosis typically involves:
Evidence of liver steatosis (through imaging or biopsy)
Presence of at least one metabolic risk factor
Exclusion of other causes of liver disease
Non-invasive tests are increasingly being used to assess disease stage and monitor progression.
Who is at risk for developing MASLD?
Risk factors include:
Obesity
Type 2 diabetes
Insulin resistance
Metabolic syndrome
Genetic predisposition
Poor diet high in processed foods and sugar
Sedentary lifestyle
Can MASLD be reversed?
Early stages of MASLD can be reversed with lifestyle modifications, particularly weight loss of 7-10% of body weight. More advanced stages may be halted or slowed, but complete reversal becomes more difficult as fibrosis progresses.
Call to Action
If you're living with obesity, diabetes, or metabolic syndrome, don’t wait. Talk to your healthcare provider about screening for liver fAT Early detection and intervention are crucial for preventing progression to more serious liver conditions.
For healthcare providers, staying updated on the evolving MASLD terminology and diagnostic criteria is essential for providing optimal patient care. Consider implementing screening protocols for at-risk patients, even those who may not fit traditional fatty liver disease profiles.
Researchers should continue exploring the complex mechanisms underlying MASLD, developing non-invasive diagnostic tools, and identifying novel therapeutic targets to address this growing global health challenge.
Together, through awareness, early intervention, and continued research, we can work toward reducing the burden of MASLD and improving outcomes for millions of affected individuals worldwide.
Related
Citations
Huang, D. Q., Wong, V. W. S., Rinella, M. E., Boursier, J., Lazarus, J. V., Yki-Järvinen, H., & Loomba, R. (2025). Metabolic dysfunction-associated steatotic liver disease in adults. Nature reviews. Disease primers, 11(1), 14. https://doi.org/10.1038/s41572-025-00599-1
Huang, D. Q., Wong, V. W., Rinella, M. E., Boursier, J., Lazarus, J. V., & Loomba, R. (2025). Metabolic dysfunction-associated steatotic liver disease in adults. Nature Reviews Disease Primers, 11(1), 1-25. https://doi.org/10.1038/s41572-025-00599-1
Wong, S. W., Yang, Y., Chen, H., Xie, L., Shen, X., Zhang, N., & Wu, J. (2025). New advances in novel pharmacotherapeutic candidates for the treatment of metabolic dysfunction-associated steatohepatitis (MASH) between 2022 and 2024. Acta Pharmacologica Sinica, 1-11. https://doi.org/10.1038/s41401-024-01466-7
Chowdhury, K., Das, D., & Huang, M. (2025). Advancing the Metabolic Dysfunction-Associated Steatotic Liver Disease Proteome: A Post-Translational Outlook. Genes, 16(3), 334. https://doi.org/10.3390/genes16030334
Iruzubieta P, Jimenez-Gonzalez C, Cabezas J, Crespo J. From NAFLD to MASLD: transforming steatotic liver disease diagnosis and management. Metab Target Organ Damage. 2025;5:10. http://dx.doi.org/10.20517/mtod.2024.143
Disclaimer
The information on this website is for informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health care provider with any questions you may have regarding a medical condition or treatment. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
About the Author:
Dr.T.S. Didwal, MD, is an experienced Internal Medicine Physician with over 30 years of practice. Specializing in internal medicine, he is dedicated to promoting wellness, preventive health, and fitness as core components of patient care. Dr. Didwal’s approach emphasizes the importance of proactive health management, encouraging patients to adopt healthy lifestyles, focus on fitness, and prioritize preventive measures. His expertise includes early detection and treatment of diseases, with a particular focus on preventing chronic conditions before they develop. Through personalized care, he helps patients understand the importance of regular health screenings, proper nutrition, exercise, and stress management in maintaining overall well-being.
