How Antidepressants Can Be a Game-Changer for Postpartum Depression"
Discover the groundbreaking research that sheds light on the transformative power of SSRI antidepressants in the treatment of postpartum depression. Explore the potential of these medications to offer new hope and relief to mothers struggling wi
DR TS DIDWAL
9/6/20238 min read


In a world where information is at our fingertips, it's crucial to rely on credible sources when seeking knowledge. One topic of immense significance, especially for new mothers, is postpartum depression. We understand the importance of providing valuable insights into this subject, and that's precisely what we aim to do in this article. Recent research has uncovered groundbreaking findings regarding the efficacy of a specific class of antidepressants, selective serotonin reuptake inhibitors (SSRIs), in the treatment of postpartum depression. Join us as we delve into this enlightening study and explore the potential benefits it offers to both mothers and their children.
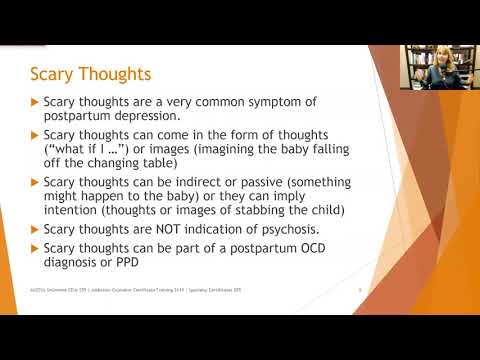
Understanding Postpartum Depression
Before delving into the study's findings, let's gain a comprehensive understanding of postpartum depression (often referred to as postnatal depression). This mental health condition affects a significant number of new mothers, with approximately 1 in 7 women experiencing its debilitating effects. It's important to note that postpartum depression can manifest up to a year following childbirth, making it a persistent concern for many women.
The Challenge of Postpartum Depression Treatment
Despite the prevalence of postpartum depression, a mere 3% of those affected opt for treatment with SSRIs. This raises an important question: Why are so few women seeking help through antidepressant therapy? One plausible explanation is the lack of concrete evidence regarding the long-term consequences of SSRI use in postpartum depression cases.
The Groundbreaking Study
A recent study, published in JAMA Network Open on August 29, has shed light on this crucial aspect of postpartum depression treatment. The research, conducted by experts at King's College London, analyzed health data from an extensive cohort of 61,081 mother-child pairs. These individuals were followed for five years after giving birth, offering an in-depth look at the effects of postpartum depression and SSRI treatment.
SSRIs: A Beacon of Hope
The findings of this study bring promising news to the forefront. Women who sought relief from postnatal depression through SSRIs, such as fluoxetine and sertraline, reported stronger relationship satisfaction and a reduced risk of depression up to five years later. This revelation is monumental, as it suggests that SSRI treatment can have a lasting positive impact on the mental health of new mothers.
A Ripple Effect on Children's Well-being
Notably, the benefits of SSRI treatment didn't stop at improving mothers' mental health. The study also uncovered a positive correlation between SSRI use and the physical and emotional well-being of their children. This aspect of the research is particularly heartening, as it underscores the potential for a profound ripple effect, benefiting not just the mothers but also the next generation.
A Closer Look at the Data
To gain a deeper understanding of the study's findings, let's break down some key insights:
Maternal Outcomes
Women experiencing more severe postnatal depression faced a higher risk of recurrent depressive episodes.
SSRI use was associated with a lower risk of maternal depression up to five years postpartum.
Relationship satisfaction was significantly higher among mothers who sought SSRI treatment.
Child Outcomes
Children born to mothers with postpartum depression often face developmental challenges, including motor and language delays.
The use of SSRIs was linked to a reduced risk of developmental delays and attention-deficit/hyperactivity (ADHD) symptoms in children.
Importantly, there was no evidence to suggest that SSRI use increased the risk of childhood psychopathology or further developmental delays.
Embracing a Path to Healing
These findings serve as a powerful reminder that postpartum depression should not be underestimated. It's a condition that can affect not only the mother's mental health but also the well-being of her children and the overall dynamics of the family.
The Importance of Seeking Help
One of the key takeaways from this research is the importance of seeking help when faced with postpartum depression. With effective treatment, mothers can better bond with their infants, strengthening.
FAQs:
What is postnatal depression, and how does it differ from other forms of depression?
Postnatal depression, also known as postpartum depression, is a type of mood disorder that affects some women after giving birth. It differs from other forms of depression in that it occurs specifically in the postpartum period, typically within the first year after childbirth. Symptoms include persistent sadness, feelings of hopelessness, fatigue, and changes in sleep and appetite.
Are antidepressants a common treatment option for postnatal depression?
Yes, antidepressants are a common and effective treatment option for postnatal depression. They are prescribed when the depression is moderate to severe or when other therapies have not produced significant improvement.
What are Selective Serotonin Reuptake Inhibitors (SSRIs), and why are they often used in postnatal depression treatment?
SSRIs are a class of antidepressant medications that work by increasing the levels of serotonin in the brain. They are commonly used in postnatal depression treatment because they are effective and have a relatively low risk of side effects.
Can antidepressants effectively treat the symptoms of postnatal depression?
Yes, antidepressants can effectively treat the symptoms of postnatal depression. They help regulate mood, reduce feelings of sadness and anxiety, and improve overall well-being.
What are the potential risks and side effects associated with using antidepressants for postnatal depression?
Common side effects of antidepressants may include nausea, dizziness, dry mouth, and changes in sleep patterns. Rarely, they can lead to more serious side effects, so it's essential to discuss potential risks with a healthcare provider.
Are there alternative treatments for postnatal depression besides antidepressants?
Yes, alternative treatments include psychotherapy (talk therapy), such as Cognitive-Behavioral Therapy (CBT) or Interpersonal Psychotherapy (IPT). Lifestyle changes, exercise, and social support can also be beneficial.
How long is the typical duration of antidepressant treatment for postnatal depression?
The duration of antidepressant treatment can vary but often lasts for several months. It's essential to follow your healthcare provider's recommendations and continue treatment until symptoms improve and for some time afterward to prevent a relapse.
Do antidepressants pose any risks to breastfeeding infants?
Some antidepressants may transfer to breast milk, but the risk to the infant is generally considered low. However, it's crucial to consult with a healthcare provider to discuss the safest options for both mother and baby during breastfeeding.
Are there specific SSRIs that are considered safer or more effective for postnatal depression?
While various SSRIs can be effective, some studies suggest that sertraline is often preferred due to its safety profile during breastfeeding and pregnancy. However, individual responses may vary, so consultation with a healthcare provider is essential.
Can psychological therapies like counseling or psychotherapy be combined with antidepressant treatment?
Yes, combining psychological therapies like counseling with antidepressant treatment can be highly effective. This approach addresses both the biological and psychological aspects of postnatal depression.
What is Interpersonal Psychotherapy (IPT), and how does it compare to antidepressant treatment for postnatal depression?
Interpersonal Psychotherapy (IPT) is a short-term psychotherapy that focuses on improving interpersonal relationships and communication. Research suggests that IPT can be as effective as antidepressant treatment for postnatal depression, and in some cases, it may be preferred.
Are there any lifestyle changes or self-help strategies that can complement antidepressant therapy in managing postnatal depression?
Lifestyle changes such as regular exercise, maintaining a healthy diet, getting adequate sleep, and seeking support from family and friends can complement antidepressant therapy and improve overall well-being.
How soon after childbirth can postnatal depression develop, and when should treatment begin?
Postnatal depression can develop at any time during the first year after childbirth, but it often appears within the first few weeks or months. Early recognition and treatment are crucial for the best outcomes.
Do women with more severe postnatal depression benefit more from antidepressant treatment?
Antidepressant treatment can be particularly beneficial for women with more severe postnatal depression, as it can help alleviate symptoms and improve daily functioning.
Are there any known long-term effects or consequences of using antidepressants during postnatal depression?
Long-term effects of antidepressant use during postnatal depression are generally favorable when monitored by a healthcare provider. The benefits of treating postnatal depression often outweigh the potential risks.
Are antidepressants safe for pregnant women who experience depression during pregnancy?
The safety of antidepressant use during pregnancy should be discussed with a healthcare provider. Some antidepressants are considered safer options during pregnancy, and the decision should weigh the risks of untreated depression against potential medication risks.
How can I determine if antidepressant treatment is the right choice for me if I'm experiencing postnatal depression?
Deciding on antidepressant treatment should be made in consultation with a healthcare provider. They can assess your symptoms, medical history, and individual circumstances to determine the most suitable treatment approach.
What steps should I take if I suspect I have postnatal depression and want to explore treatment options?
If you suspect you have postnatal depression, reach out to a healthcare provider or mental health professional. They can provide a thorough assessment and guide you through available treatment options.
Are there support groups or resources available for women dealing with postnatal depression?
Yes, there are numerous support groups, online communities, and resources available for women experiencing postnatal depression. These can provide valuable emotional support and information.
What do the latest research and medical guidelines say about the use of antidepressants in postnatal depression treatment?
The latest research and medical guidelines generally support the use of antidepressants as a valuable treatment option for postnatal depression, especially in cases of moderate to severe depression. However, individualized treatment plans are essential, and ongoing research may influence recommendations.
RESEARCH:
Postpartum depression may last for years. A study published in the journal JAMA Network Open found that about 5% of women reported persistently high levels of postpartum depression symptoms for three years after giving birth. This suggests that longer screening periods after birth may be needed to help more women with postpartum depression get treatment.
Risk factors for postpartum depression vary by race and ethnicity. A study published in the journal Depression and Anxiety found that black women are more likely to experience postpartum depression than white women. The study also found that Hispanic women are more likely to experience postpartum depression than non-Hispanic white women. The reasons for these disparities are not fully understood, but they may be due to a combination of factors, such as socioeconomic status, access to healthcare, and cultural beliefs about motherhood.
Postpartum depression can be treated with medication and therapy. The most common treatments for postpartum depression are medication and therapy. Medications such as selective serotonin reuptake inhibitors (SSRIs) and SNRIs can help to relieve the symptoms of depression. Therapy, such as cognitive-behavioral therapy (CBT), can help women understand and manage their thoughts and feelings about their postpartum experience.
Postpartum depression can have a long-term impact on mothers and babies. Postpartum depression can hurt the mother-baby relationship, as well as the mother's physical and mental health. Children of mothers with postpartum depression are also at an increased risk of developing mental health problems later in life.
There is a growing movement to destigmatize postpartum depression. In recent years, there has been a growing movement to destigmatize postpartum depression. This has led to more women seeking help for the condition and more research being conducted on its causes and treatments.
New technologies are being developed to help diagnose and treat postpartum depression. Researchers are developing new technologies to help diagnose and treat postpartum depression. For example, one study is using wearable devices to track heart rate and sleep patterns, which can be used to identify women who are at risk for postpartum depression.
The role of social support in postpartum depression is being explored. Researchers are also exploring the role of social support in postpartum depression. Studies have shown that women with strong social support networks are less likely to experience postpartum depression.
The impact of postpartum depression on the workplace is being studied. Postpartum depression can have a significant impact on the workplace. Women with postpartum depression may miss work, be less productive, and have difficulty making decisions. Employers are starting to recognize the importance of providing support to employees with postpartum depression.
The role of fathers in postpartum depression is being examined. Fathers can also play a role in supporting mothers with postpartum depression. Studies have shown that fathers who are supportive of their partners can help to reduce the severity of the depression.
The prevention of postpartum depression is a growing area of research. Researchers are working to develop strategies to prevent postpartum depression. One promising approach is to provide preventive interventions to women who are at risk for the condition.
RELATED:
NOVEL ADepT APPROACH FOR ANHEDONIC DEPRESSION | Healthnewstrend
Extended Antidepressant Therapy: A Game-Changer in Bipolar Disorder | Healthnewstrend
VIDEO COURTESY:
Postpartum Depression after Pregnancy
Doc Snipes