How does obesity impact brain function and increase dementia risk?
Discover the alarming connection between obesity, brain function, and dementia. Learn how excess weight impacts cognitive abilities and increases the risk of neurodegenerative diseases. Find out about the latest research and potential prevention strategies.
DR T S DIDWAL MD
8/7/20247 min read
Obesity is increasingly linked to cognitive decline and dementia. While BMI is often used, body composition and fat distribution are more accurate measures. Research shows obesity impacts brain function through inflammation, disrupting communication pathways, and affecting crucial brain regions. Weight loss can improve cognitive function. However, the "obesity paradox" suggests being overweight in older adults might be linked to lower dementia risk, likely due to factors like unintentional weight loss signaling underlying health issues or protective effects of extra body fat. Addressing obesity is crucial for both physical and mental well-being, with early intervention and personalized care being key. Exploring the Link Between Obesity and Cognitive Function Obesity, typically defined as having a body mass index (BMI) of 30 or higher, is a growing global health concern. However, BMI alone doesn't capture differences in body composition or fat distribution. Central or abdominal obesity, measured by waist circumference, is particularly relevant to cognitive effects. Cognitive function includes mental abilities like memory, attention, executive function, information processing, and language skills. Research shows obesity affects multiple cognitive domains, with effects varying based on factors like age and obesity duration.
Keypoints
Obesity is linked to cognitive decline: Excess body weight, particularly in midlife, can negatively impact brain health.
Inflammation is a key factor: Chronic inflammation caused by obesity disrupts brain communication pathways and damages brain regions.
Cognitive function impacts weight management: Brain health plays a role in successful weight loss efforts.
Weight loss can improve cognitive function: Reducing excess weight can enhance memory, attention, and decision-making abilities.
Body composition matters: Measuring body fat distribution (not just BMI) is crucial for understanding obesity's impact on the brain.
The "obesity paradox" is complex: Being overweight in older adults might be linked to lower dementia risk, but more research is needed.
Early intervention and personalized care are essential: Addressing obesity early and tailoring treatments to individual needs is crucial for brain health.
The Obesity-Cognition Link: Key Findings
Epidemiological evidence links obesity to poorer cognitive performance. Key findings include:
Midlife obesity increases dementia risk later in life.
Higher BMI correlates with reduced brain volume in areas like the frontal lobes and hippocampus.
Obese individuals perform worse on tests of executive function and processing speed.
Weight loss interventions can improve cognitive performance in obese adults.
However, this relationship is complex, with conflicting findings, especially in older adults. Let's explore two studies that shed light on this connection.
Scientific Validation
Study 1: Obesity, Inflammation, and Brain Function
Recent research highlights obesity's impact on brain function through chronic, low-grade inflammation. Le Thuc's review in Nature Metabolism examines how obesity-induced inflammation disrupts brain function, elevating the risk of cognitive impairments, including Alzheimer's and dementia.
Chronic Inflammatory State
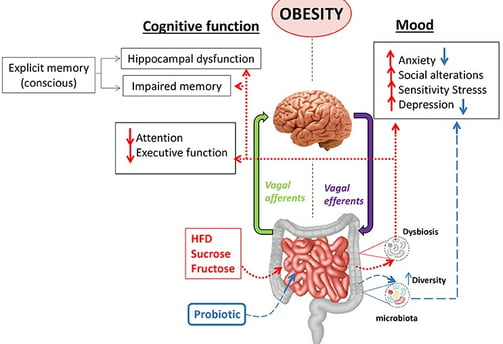
Obesity triggers excessive fat accumulation, causing persistent inflammation that affects the whole body. This constant immune activation disrupts physiological processes and impairs communication between body systems and the brain. Inflammation disrupts key pathways, including the blood-brain barrier (BBB), glymphatic system, and meninges. The compromised BBB allows pro-inflammatory molecules into the brain, exacerbating neuronal damage and impairing cognitive function. Inflammation also reduces the glymphatic system's efficiency, leading to the accumulation of metabolic waste products like amyloid-beta, associated with Alzheimer’s disease.
Impact on Brain Regions
Obesity-induced inflammation affects brain regions like the hypothalamus and hippocampus, which are crucial for energy homeostasis and cognition. This increases the risk of cognitive impairment and neurodegenerative diseases. The relationship between obesity and cognitive impairment is bidirectional. Cognitive impairment can worsen obesity, creating a cycle where both conditions reinforce each other.
Potential Interventions
Addressing obesity-induced inflammation requires a multifaceted approach:
Lifestyle Modifications: A healthy diet and regular physical activity can reduce inflammation and improve cognitive function.
Medical Interventions: In severe cases, medications or surgical interventions may be necessary. Anti-inflammatory treatments can protect brain function.
Cognitive Training: Engaging in brain-stimulating activities can improve cognitive function and counteract inflammation effects.
Stress Management: Techniques like mindfulness and meditation can reduce chronic stress and inflammation.
Early Intervention: Regular health check-ups and cognitive assessments can detect issues early, allowing for timely intervention.
Study 2: Obesity and Brain Health: A Complex Relationship
Obesity is increasingly linked to cognitive decline and dementia. While often defined by BMI, more accurate measures consider body composition and fat distribution. Beyond physical implications, obesity is associated with health issues like type 2 diabetes, cancer, and cognitive deficits. Research published in Medicina indicates a strong correlation between obesity and impaired cognitive function, particularly in memory, attention, and decision-making. Weight loss interventions have shown promise in improving cognitive performance in obese individuals.
Obesity and Dementia
Obesity increases Alzheimer's disease risk, but the relationship is complex. Some studies suggest a protective effect of obesity in older populations, potentially due to sarcopenic obesity (loss of muscle mass with excessive fat) and BMI's limitations. Neuroimaging studies link obesity to structural brain changes, contributing to cognitive decline. Factors like childhood maltreatment, hormone imbalances, and chronic inflammation play a role. Researchers use techniques like DXA, MRI, pQCT, and air displacement plethysmography to assess body composition and brain structure.
Potential Mechanisms
Several biological pathways have been proposed to explain how obesity might influence cognitive function:
Inflammation: Excess body fat, especially visceral fat, promotes chronic low-grade inflammation. Pro-inflammatory molecules can cross the blood-brain barrier and potentially disrupt neural function.
Altered hormone signaling: Obesity affects levels of hormones like leptin and insulin, which play roles in brain health and cognition. For instance, inefficient leptin signaling has been linked to changes in hippocampus structure and decreased memory performance.
Vascular effects: Obesity is a risk factor for conditions like hypertension and diabetes, which can damage blood vessels in the brain over time.
Brain-derived neurotrophic factor (BDNF): Some research suggests obesity is associated with reduced levels of BDNF, a protein important for neuroplasticity and cognitive function.
Metabolic changes: Obesity may alter brain glucose metabolism, potentially affecting cognitive processes.
The Obesity Paradox in Older Adults
While midlife obesity is generally associated with increased dementia risk, the relationship becomes more complex in older adults. Some studies have found that being over While midlife obesity is generally associated with increased dementia risk, the relationship becomes more complex in older adults. Some studies have found that being overweight or mildly obese in later life is actually associated with a lower risk of cognitive decline – a phenomenon known as the "obesity paradox."
Several factors may contribute to this paradox:
Unintentional weight loss in older adults can be a sign of underlying health issues or early dementia
Extra body fat may provide some protective effects in very old age
BMI becomes a less accurate measure of adiposity in older adults due to changes in body composition
This complexity highlights the need for more nuanced measures of body composition when studying obesity's effects, especially in older populations.
Implications for Public Health and Clinical Practice
The evidence linking obesity to cognitive decline has important implications:
Early Intervention: Preventing and treating childhood obesity is critical.
Cognitive Benefits of Weight Loss: Weight loss can improve cognitive function, motivating lifestyle changes.
Brain Health in Weight Management: Cognitive function plays a role in successful weight management.
Personalized Approaches: Obesity's complex relationship with cognition requires personalized health management.
Comprehensive Health Assessments: Cognitive screening may be valuable in obesity treatment, and vice versa.
Conclusion
Obesity's relationship with cognitive function is complex and multifaceted. Excess body fat, especially in midlife, may negatively impact brain health and increase cognitive decline and dementia risk. However, effects vary based on age, fat distribution, and metabolic complications. Addressing obesity may protect both physical and mental well-being, highlighting the importance of maintaining a healthy body composition for preserving cognitive function across the lifespan.
Faqs
1. Q: Does obesity affect brain function? Yes, research suggests obesity is associated with reduced cognitive function, particularly in areas like executive function, memory, and processing speed. It may also lead to structural changes in the brain over time.
2. Q: Can losing weight improve cognitive function? Several studies indicate that intentional weight loss in obese adults can lead to improvements in cognitive performance, particularly in areas like attention, memory, and executive function.
3. Q: Is obesity linked to dementia risk? Yes, obesity in midlife has been associated with an increased risk of developing dementia later in life. However, the relationship becomes more complex in older adults.
4. Q: How does obesity affect the brain in teenagers? Research has shown that obesity in adolescents is associated with subtle changes in brain structure, including cortical thinning in specific regions and reduced integrity of white matter tracts. These changes may affect academic performance.
5. Q: What is the obesity paradox in cognitive function? The obesity paradox refers to findings that being overweight or mildly obese in older age is sometimes associated with a lower risk of cognitive decline, contrary to the increased risk seen in midlife obesity.
6. Q: Is there a two-way relationship between obesity and cognitive function? Yes, studies have found a bidirectional relationship. Obesity can lead to cognitive decline over time, while better cognitive function (especially executive function) may help prevent future weight gain.
7. Q: How does body fat affect the brain? Excess body fat may impact the brain through various mechanisms, including inflammation, altered hormone signaling, vascular effects, and changes in levels of proteins important for brain health like BDNF.
8. Q: Is BMI the best way to measure obesity when studying cognitive effects? While BMI is commonly used, it has limitations. Other measures like waist circumference or more advanced techniques for assessing body composition may provide more accurate information, especially when studying cognitive effects.
Journal References
1. Le Thuc, O. (2024). Obesity-induced inflammation: Connecting the periphery to the brain. Nature Metabolism, 6(7), 1237-1252. https://doi.org/10.1038/s42255-024-01079-8
2 . Sui, S. X., & Pasco, J. A. (2020). Obesity and Brain Function: The Brain-Body Crosstalk. Medicina (Kaunas, Lithuania), 56(10), 499. https://doi.org/10.3390/medicina56100499
Image credit: https://www.frontiersin.org/files/Articles/329519/fnins-12-00155-HTML/image_m/fnins-12-00155-g002.jpg
Related
https://healthnewstrend.com/ibs-and-the-brain-low-dose-antidepressants-and-the-brain-gut-axis
https://healthnewstrend.com/exercise-as-medicine-can-it-overcome-depression-and-anxiety
Disclaimer
The information on this website is for informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition or treatment. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
