How Exercise Rewires Your Cells to Protect Muscle Health
Discover how exercise acts as medicine by activating cellular pathways that protect muscle health and prevent atrophy, aging, and disease-related loss
DR T S DIDWAL MD
4/11/202510 min read
Molecular and Cellular Mechanisms Underpinning Exercise Benefits in Aging Muscle
As muscle loss and frailty accelerate with age, exercise remains the most effective intervention to preserve muscle mass, strength, and resilience. This article explores the molecular biology behind exercise-induced adaptations in skeletal muscle, with a focus on aging populations.
Key Mechanisms:
Mitochondrial Health: Exercise improves mitochondrial biogenesis, dynamics, and efficiency through activation of PGC-1α, AMPK, and SIRT1, countering the age-related decline in mitochondrial quality.
Stress Response & Proteostasis: Physical activity upregulates cellular defense proteins such as HSP70 and SESN2, enhancing the muscle’s ability to manage oxidative stress, DNA damage, and misfolded proteins.
Autophagy & Muscle Quality: Exercise restores autophagic flux via FOXO3a, improving the clearance of damaged organelles and maintaining cellular homeostasis.
Inflammation & Redox Balance: It modulates systemic and intramuscular inflammation, reducing chronic low-grade inflammation ("inflammaging") through Nrf2, IL-6, and mitokine pathways.
Neuromuscular Integrity: Training protects motor neurons, preserves neuromuscular junctions, and enhances coordination—key to preventing sarcopenic falls and disability.
Exercise induces a coordinated cellular stress response that rejuvenates aging muscle at the mitochondrial, transcriptional, and proteomic levels. These adaptations slow sarcopenia, extend healthspan, and offer a powerful non-pharmacologic strategy for combating age-related decline.
Far beyond strength and endurance, exercise is a systemic modulator of aging biology—targeting hallmarks of aging at the molecular level and positioning itself as a cornerstone of precision geroscience.
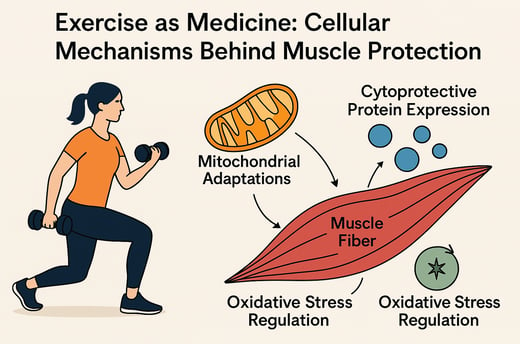
Exercise Preconditioning: Molecular Mechanisms and Benefits for Muscle Health
Exercise preconditioning is emerging as a powerful, non-pharmacological strategy to combat muscle atrophy, especially in aging populations. This scientifically backed approach involves performing targeted physical activity before potential muscle stressors—such as immobility, aging, or illness—to build a protective molecular shield in skeletal muscle. At the core of its benefits are mitochondrial adaptations, cytoprotective protein expression (like HSP72, SOD2, PGC-1α, and AMPK), and oxidative stress regulation, which collectively improve energy metabolism, resilience, and muscle repair.
Recent research highlights that exercise enhances mitochondrial density, boosts capillarization, and promotes muscle strength and mass, especially when combined with neuromuscular electrical stimulation (NMES). Multi-omic studies further confirm that exercise triggers profound changes across tissues—benefiting everything from cardiovascular health to immune regulation.
For optimal muscle health, experts recommend multicomponent training—including resistance, aerobic, flexibility, and cognitive tasks—tailored to individual needs. Despite the clear benefits, exercise remains underutilized in medical care, especially for older adults.
The takeaway? Exercise is not just prevention—it’s precision medicine for muscle health. Implementing personalized, science-driven exercise regimens can significantly slow aging, reduce disease burden, and enhance quality of life.
The Universal Challenge of Aging and the Exercise Solution
Aging is an inevitable biological process characterized by progressive physiological deterioration and functional decline. This natural progression increases our vulnerability to diseases and, ultimately, mortality. However, emerging research suggests that lifestyle factors, particularly physical activity and exercise, significantly modulate aging phenotypes.
Recent consensus indicates that exercise can prevent or ameliorate lifestyle-related diseases, extend health span, enhance physical function, and reduce the burden of non-communicable chronic diseases including cardiometabolic disease, cancer, musculoskeletal and neurological conditions, and chronic respiratory diseases.
What makes exercise particularly fascinating is its influence on the cellular and molecular drivers of biological aging, effectively slowing aging rates—a foundational aspect of geroscience. This positions physical activity as both preventive medicine and a therapeutic agent in pathological states.
Understanding Skeletal Muscle Atrophy
Skeletal muscle atrophy, characterized by the loss of muscle mass and function, represents a significant health concern that can result from various factors:
Disuse (sedentary behavior, immobilization)
Aging (sarcopenia)
Disease (cancer cachexia, heart failure)
Drug-induced muscle wasting (certain medications)
The consequences extend beyond mere physical limitations, affecting metabolic health, independence, and quality of life. This makes effective interventions against muscle atrophy a critical area of research focus.
Exercise Preconditioning: A Powerful Protective Strategy
One particularly promising approach is exercise preconditioning—a form of exercise training performed before exposure to harmful threats. Research has shown that this preemptive strategy induces notable remodeling and extensive biochemical adaptations in skeletal muscle, creating a protective phenotype in muscle fibers.
Cellular Mechanisms of Protection
Several key mechanisms contribute to the protective effects of exercise on skeletal muscle fibers:
Mitochondrial adaptations: Enhanced mitochondrial function, biogenesis, and quality control
Cytoprotective protein expression: Upregulation of proteins such as:
HSP72 (Heat Shock Protein 72)
SOD2 (Superoxide Dismutase 2)
SESN2 (Sestrin 2)
PGC-1α (Peroxisome proliferator-activated receptor gamma coactivator 1-alpha)
AMPK (AMP-activated protein kinase)
Oxidative stress regulation: Improved antioxidant defense systems
These adaptations collectively confer resilience against various forms of muscle atrophy, highlighting the potential of exercise preconditioning as a non-pharmacological intervention for preserving muscle mass and function.
Insights from Recent Research
Study 1: Effects of Exercise Training on Mitochondrial and Capillary Growth
Mølmen, Almquist, and Skattebo (2025) conducted a systematic review and meta-regression examining how exercise training affects mitochondrial and capillary growth in human skeletal muscle. This comprehensive analysis provides crucial insights into the adaptive responses to exercise at the cellular level.
Key Findings:
Exercise training significantly increases mitochondrial density and function
Enhanced capillarization improves oxygen and nutrient delivery to muscle fibers
These adaptations correlate with improved aerobic capacity and metabolic health
The magnitude of adaptations appears dose-dependent, with higher training volumes generally yielding greater benefits
These findings underscore the importance of mitochondrial health and adequate muscle perfusion in maintaining optimal muscle function and preventing atrophy.
Study 2: Comparing Conventional Resistance Training with Combined NMES
The second study compared strength and muscle mass development between conventional resistance training (RT) and a combined approach of resistance training with neuromuscular electrical stimulation (RT + NMES).
Methodology:
Systematic search of multiple databases
Inclusion of randomized controlled trials comparing RT alone versus RT + NMES
Analysis of strength gains and muscle mass development
Calculation of effect sizes using standard mean difference (SMD)
Results:
The combined RT + NMES approach showed superior effects for strength gain (SMD: 0.31; 95% CI 0.13–0.49; p = 0.02)
Similar advantages were observed for muscle mass development (SMD: 0.26; 95% CI 0.04–0.49; p = 0.02)
Lower heterogeneity was found in the muscle mass analysis (I² = 21.45%) compared to strength gain (I² = 73.05%)
Practical Implication: Incorporating neuromuscular electrical stimulation into resistance training protocols may represent a more effective strategy to improve muscle strength and mass. This combined approach could be particularly beneficial for populations at high risk of muscle atrophy, such as older adults or patients undergoing rehabilitation.
Study 3: Molecular Transducers of Physical Activity Consortium Research
The third study presents groundbreaking work from the Molecular Transducers of Physical Activity Consortium, which profiled temporal changes across multiple molecular levels in response to endurance exercise training.
Study Design:
Comprehensive profiling in male and female Rattus norvegicus (rats)
Eight-week endurance exercise training protocol
Analysis of transcriptome, proteome, metabolome, lipidome, phosphoproteome, acetylproteome, ubiquitylproteome, epigenome, and immunome
Samples from whole blood, plasma, and 18 solid tissues
Key Insights:
The resulting data compendium encompasses 9,466 assays across 19 tissues, 25 molecular platforms, and 4 training time points
Thousands of shared and tissue-specific molecular alterations were identified
Sex differences were observed in multiple tissues
Widespread regulation of immune, metabolic, stress response, and mitochondrial pathways was documented
Relevance to Human Health: Many of the observed changes were directly relevant to human health conditions, including:
Non-alcoholic fatty liver disease
Inflammatory bowel disease
Cardiovascular health
Tissue injury and recovery mechanisms
This extensive multi-omic and multi-tissue analysis provides unprecedented insights into the adaptive responses to endurance training at the molecular level.
Study 4: The Consensus on Exercise for Aging Adults
This recent study offers a comprehensive consensus on the integration of physical activity into health promotion, disease prevention, and management strategies for older adults.
Key Points:
Structured exercise prescriptions should be customized and monitored like any other medical treatment
Current guidelines recommend a multifaceted exercise regimen including aerobic, resistance, balance, and flexibility training
Progressive resistance training (PRT) is particularly important for maintaining functional capacity in older adults
Multicomponent exercise interventions that include cognitive tasks enhance both physical and cognitive function
Economic analyses support the cost-effectiveness of exercise programs for older adults
Implementation Challenges: Despite the well-documented benefits, exercise remains underutilized in medical practice for older people. Many healthcare professionals, including geriatricians, need more training to incorporate exercise directly into patient care. This represents a significant opportunity for improvement in geriatric healthcare delivery.
The Science Behind Exercise-Induced Muscle Protection
Mitochondrial Adaptations: The Powerhouse Effect
Mitochondria, often called the powerhouses of the cell, play a crucial role in exercise-induced muscle protection. Regular exercise stimulates mitochondrial biogenesis—the formation of new mitochondria—and enhances their function through:
Increased expression of PGC-1α, a master regulator of mitochondrial biogenesis
Enhanced mitochondrial dynamics (fusion and fission processes)
Improved mitochondrial quality control through mitophagy (removal of damaged mitochondria)
Optimized electron transport chain function
These adaptations collectively improve energy production efficiency while reducing the generation of harmful reactive oxygen species (ROS), creating a more resilient cellular environment.
Cytoprotective Protein Expression: The Molecular Shields
Exercise preconditioning induces the expression of several protective proteins that shield muscle fibers from various stressors:
HSP72 (Heat Shock Protein 72): Acts as a molecular chaperone, preventing protein misfolding and aggregation during stress conditions
SOD2 (Superoxide Dismutase 2): Neutralizes superoxide radicals, protecting against oxidative damage
SESN2 (Sestrin 2): Regulates cellular metabolism and stress responses, while also inhibiting mTOR when appropriate
PGC-1α: Beyond mitochondrial biogenesis, it enhances overall cellular resilience
AMPK (AMP-activated protein kinase): Serves as a cellular energy sensor that promotes ATP production while inhibiting energy-consuming processes during stress
The coordinated action of these proteins establishes a robust defense system against various forms of cellular stress that could otherwise lead to muscle atrophy.
Oxidative Stress Regulation: Finding the Balance
Exercise induces a hormetic response to oxidative stress—a beneficial adaptation to moderate levels of a stressor that would be harmful at higher doses. Regular physical activity:
Enhances antioxidant enzyme systems (catalase, glutathione peroxidase)
Increases redox signaling sensitivity
Improves the efficiency of damage repair mechanisms
Establishes a more favorable redox balance
This adaptive response to exercise-induced oxidative stress creates a cellular environment that can better withstand subsequent challenges, whether from disuse, aging, disease, or pharmaceutical interventions.
Practical Applications: Translating Research into Action
Exercise Prescription for Preventing Muscle Atrophy
Based on the consolidated research, an effective exercise regimen to prevent muscle atrophy should include:
Resistance Training: 2-3 sessions per week, focusing on:
Multi-joint exercises (squats, deadlifts, push-ups)
Progressive overload (gradually increasing resistance)
2-3 sets of 8-12 repetitions per exercise
Aerobic Exercise: 150-300 minutes per week of moderate-intensity or 75-150 minutes of vigorous-intensity activity, including:
Walking, cycling, swimming
High-intensity interval training (HIIT) for time-efficient benefits
Multicomponent Training: Combining elements of:
Resistance training
Aerobic exercise
Balance and flexibility work
Cognitive tasks (dual-task training)
Consider Adjunctive Approaches: For enhanced benefits:
Neuromuscular electrical stimulation (NMES) combined with resistance training
Nutritional support (adequate protein intake, vitamin D)
Special Considerations for Aging and Clinical Populations
For older adults and those with clinical conditions:
Individualized Assessment: Conduct thorough evaluations of:
Functional capacity
Medical contraindications
Personal preferences
Progressive Approach: Start with lower intensities and volumes, gradually increasing as tolerance improves
Supervision: Provide proper instruction and monitoring, especially during initial phases
Adherence Strategies: Implement approaches to enhance long-term compliance:
Group-based training
Enjoyable activities
Regular feedback on progress
Social support mechanisms
FAQs About Exercise and Muscle Health
Q1: How much exercise is needed to prevent muscle atrophy?
A: Current guidelines recommend at least 150 minutes of moderate-intensity aerobic activity plus two or more days of muscle-strengthening activities per week. However, even smaller amounts of activity provide benefits, making "something better than nothing" a practical starting point for sedentary individuals.
Q2: Can exercise reverse existing muscle atrophy?
A: Yes, in many cases. Progressive resistance training, particularly when combined with adequate protein intake, has been shown to reverse muscle atrophy in various populations, including older adults with sarcopenia and patients recovering from disuse atrophy.
Q3: Is neuromuscular electrical stimulation (NMES) safe for everyone?
A: While generally safe, NMES has some contraindications, including pregnancy, epilepsy, cardiac pacemakers, and certain skin conditions. Always consult a healthcare provider before starting NMES treatment, especially for clinical populations.
Q4: How does exercise protect against age-related muscle loss?
A: Exercise combats age-related muscle loss through multiple mechanisms: stimulating protein synthesis, reducing inflammation, enhancing mitochondrial function, improving insulin sensitivity, optimizing hormonal environment, and activating satellite cells (muscle stem cells) necessary for repair and growth.
Q5: Can too much exercise cause muscle damage?
A: Yes, excessive exercise without adequate recovery can lead to overtraining syndrome, which may include muscle damage, reduced performance, and systemic inflammation. Proper periodization (cycling training intensity and volume) is essential for long-term muscle health.
Key Takeaways
Exercise preconditioning creates a protective phenotype in muscle fibers that helps prevent atrophy from disuse, aging, disease, and certain medications.
Key molecular mechanisms behind exercise-induced muscle protection include mitochondrial adaptations, cytoprotective protein expression, and improved oxidative stress regulation.
Combined approaches, such as resistance training with neuromuscular electrical stimulation, may offer superior benefits for muscle strength and mass compared to conventional resistance training alone.
Comprehensive exercise programs should include resistance, aerobic, balance, and flexibility components, particularly for older adults.
Sex differences exist in molecular responses to exercise, highlighting the need for gender-specific research and potentially tailored exercise prescriptions.
Multicomponent exercise interventions that include cognitive tasks significantly enhance both physical and cognitive function in aging populations.
Exercise prescription should be personalized, considering individual variability in adaptation responses, especially in older adult cohorts.
Implementation gaps remain in integrating exercise into mainstream geriatric care, despite strong evidence supporting its benefits.
Call to Action
The evidence is clear: exercise represents one of the most powerful tools we have to combat muscle atrophy and promote healthy aging. Whether you're a healthcare professional, researcher, fitness enthusiast, or someone concerned about maintaining muscle health throughout life, here's how you can apply these insights:
For healthcare providers: Consider exercise as a first-line intervention for preventing and treating muscle atrophy. Familiarize yourself with evidence-based exercise prescriptions and refer patients to qualified exercise professionals when appropriate.
For researchers: Continue investigating the molecular mechanisms of exercise adaptation, with particular focus on personalized approaches and implementation strategies that bridge laboratory findings and clinical practice.
For individuals: Start or maintain a comprehensive exercise program that includes both resistance and aerobic components. Remember that consistency trumps intensity, especially when beginning, and that benefits accrue even from modest activity levels.
For policy makers: Support initiatives that integrate exercise into healthcare systems, from reimbursement for exercise programs to training for healthcare professionals on exercise prescription.
By collectively embracing the science of exercise preconditioning, we can take significant strides toward a future where muscle health is preserved throughout the lifespan, enhancing quality of life and reducing the burden of age-related decline.
Ready to take the next step in your exercise journey? Consult with a qualified exercise professional to develop a personalized program that addresses your specific needs and goals.
Remember: The best exercise program is the one you'll actually do consistently!
Related Articles
Rebuild Strength After 60: Science-Backed Training to Reverse Sarcopenia
Citations
Zhou, X., Li, S., Wang, L., Wang, J., Zhang, P., & Chen, X. (2025). The emerging role of exercise preconditioning in preventing skeletal muscle atrophy. Frontiers in physiology, 16, 1559594. https://doi.org/10.3389/fphys.2025.1559594
Narvaez, G., Apaflo, J., Wagler, A. et al. The additive effect of neuromuscular electrical stimulation and resistance training on muscle mass and strength. Eur J Appl Physiol (2025). Narvaez, G., Apaflo, J., Wagler, A. et al. The additive effect of neuromuscular electrical stimulation and resistance training on muscle mass and strength. Eur J Appl Physiol (2025). https://doi.org/10.1007/s00421-024-05700-2
Mølmen, K. S., Almquist, N. W., & Skattebo, Ø. (2025). Effects of Exercise Training on Mitochondrial and Capillary Growth in Human Skeletal Muscle: A Systematic Review and Meta-Regression. Sports medicine (Auckland, N.Z.), 55(1), 115–144. https://doi.org/10.1007/s40279-024-02120-2
Izquierdo, M., de Souto Barreto, P., Arai, H., Bischoff-Ferrari, H. A., Cadore, E. L., Cesari, M., Chen, L. K., Coen, P. M., Courneya, K. S., Duque, G., Ferrucci, L., Fielding, R. ., … Fiatarone Singh, M. A. (2025). Global consensus on optimal exercise recommendations for enhancing healthy longevity in older adults (ICFSR). The journal of nutrition, health & aging, 29(1), 100401. https://doi.org/10.1016/j.jnha.2024.100401
(2024). Temporal dynamics of the multi-omic response to endurance exercise training. Nature, 629(8010), 174-183. https://doi.org/10.1038/s41586-023-06877-w
Disclaimer
The information on this website is for informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health care provider with any questions you may have regarding a medical condition or treatment.Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
About the Author:
Dr.T.S. Didwal, MD, is an experienced Internal Medicine Physician with over 30 years of practice. Specializing in internal medicine, he is dedicated to promoting wellness, preventive health, and fitness as core components of patient care. Dr. Didwal’s approach emphasizes the importance of proactive health management, encouraging patients to adopt healthy lifestyles, focus on fitness, and prioritize preventive measures. His expertise includes early detection and treatment of diseases, with a particular focus on preventing chronic conditions before they develop. Through personalized care, he helps patients understand the importance of regular health screenings, proper nutrition, exercise, and stress management in maintaining overall well-being.
