IBS and NAFLD Correlation: Unraveling the Gut-Liver Connection
Learn about the correlation between irritable bowel syndrome (IBS) and non-alcoholic fatty liver disease (NAFLD), and how the gut-liver connection plays a role in their development. Discover the latest research and potential treatment options in this comprehensive 2023 guide.
DR T S DIDWAL ,MD
9/21/20238 min read
In the world of health and wellness, acronyms like IBS and NAFLD may seem like alphabet soup, but understanding their correlation can be a key piece in the puzzle of our overall well-being. Irritable Bowel Syndrome (IBS) and Non-Alcoholic Fatty Liver Disease (NAFLD) are two common conditions that can affect individuals independently, but research suggests there might be a connection between them. In this article, we'll dive into the intricacies of IBS and NAFLD, exploring their correlation and what it means for your health.
What is IBS?
IBS, or Irritable Bowel Syndrome, is a gastrointestinal disorder characterized by abdominal pain, bloating, and changes in bowel habits. It affects millions of people worldwide, often leading to discomfort and a reduced quality of life. Symptoms can vary from person to person, making it a perplexing condition to diagnose and manage.
While the exact cause of IBS remains elusive, factors like diet, stress, and gut microbiota are thought to play a role. The number of symptoms, which can range from constipation to diarrhea, can be a daily challenge for those living with IBS.
What is NAFLD?
On the flip side, NAFLD, or Non-Alcoholic Fatty Liver Disease, is a condition where fat accumulates in the liver, resembling the damage caused by excessive alcohol consumption but occurring in people who don't drink excessively. NAFLD is often associated with obesity, diabetes, and metabolic syndrome, and it can progress to more severe liver conditions if left unchecked.
This condition often develops silently, with few noticeable symptoms in its early stages. However, as it progresses, it can lead to liver inflammation, cirrhosis, and even liver cancer.
The Puzzle: IBS and NAFLD Connection
Now, let's explore the perplexing correlation between these two seemingly unrelated conditions. Recent studies have indicated that there is a higher prevalence of IBS in individuals with NAFLD and vice versa. This raises a perplexing question: Is there a common thread that connects the gut and the liver?
Some research suggests that both conditions may share common risk factors, such as obesity and poor dietary choices. Additionally, they may both be influenced by chronic inflammation, which is a significant contributor to the burstiness of symptoms in IBS and the progression of NAFLD.
Gut Health and Liver Function
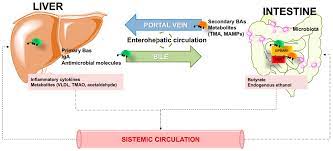
To understand this connection further, we need to delve into the concept of the gut-liver axis. This intricate network of communication between the gut and the liver plays a vital role in maintaining overall health. Changes in the gut microbiota, which can occur in IBS, may influence liver function and contribute to the development of NAFLD.
Inflammation: The Culprit?
One of the most perplexing aspects of the IBS-NAFLD correlation is the role of inflammation. Studies have shown that both conditions involve chronic inflammation, although they manifest in different ways. IBS is characterized by gastrointestinal inflammation, leading to abdominal discomfort, while NAFLD involves inflammation within the liver.
Is inflammation the bridge connecting these two conditions? It's a perplexing question, but emerging research suggests that reducing inflammation in the gut through dietary and lifestyle changes might benefit both IBS and NAFLD patients.
Dietary Habits and Their Impact
Dietary choices can significantly impact the burstiness and severity of symptoms in both IBS and NAFLD. For IBS patients, certain foods can trigger flare-ups, leading to discomfort and distress. Similarly, in NAFLD, a high intake of sugary and fatty foods can exacerbate liver damage.
To address both conditions, it's essential to adopt a gut-friendly and liver-friendly diet. Incorporating fiber-rich foods, lean proteins, and plenty of fruits and vegetables can be a good starting point. However, specific dietary recommendations may vary depending on individual symptoms and needs.
Managing IBS for Liver Health
If you have IBS and are concerned about its potential impact on your liver, there are steps you can take to manage your symptoms and potentially mitigate the risk to your liver. Lifestyle changes, such as stress reduction techniques, regular exercise, and adequate hydration, can help alleviate IBS symptoms and promote overall well-being.
NAFLD Management and IBS Considerations
Conversely, for those with NAFLD, managing the condition requires attention to diet and lifestyle. However, it's crucial to consider how these strategies may affect IBS symptoms. For example, some dietary changes recommended for NAFLD, like reducing fatty foods, may also be beneficial for IBS. Consulting a healthcare professional for personalized guidance is essential.
Lifestyle Adjustments
Beyond medical intervention, making certain lifestyle adjustments can positively impact both IBS and NAFLD. Regular exercise, for instance, can promote gut motility and improve liver function. Stress management techniques, such as meditation or yoga, can also help reduce the burstiness of IBS symptoms and potentially mitigate inflammation.
The Mind-Gut Connection
The impact of mental health on IBS and NAFLD should not be underestimated. Stress, anxiety, and depression can exacerbate symptoms in both conditions. Therefore, addressing your mental well-being is a crucial aspect of managing IBS and NAFLD.
Latest Research:
Bridging the Gap: Investigating NAFLD and IBS Risk
To shed light on this compelling connection, researchers embarked on a large-scale population-based cohort study with a long-term follow-up of 0.4 million adults in the United Kingdom. Their goal was to investigate the association between the degree of non-alcoholic fatty liver and the presence of NAFLD with the risk of incident IBS.
The results of this ambitious study were nothing short of groundbreaking. Participants with the highest quartile of the fatty liver index had a 21% increased risk of developing IBS, while those with a confirmed diagnosis of NAFLD faced a 13% higher risk of encountering IBS. Intriguingly, this positive association was particularly pronounced in females, raising questions about potential gender-specific factors at play.
Unraveling the Mysteries: Potential Mechanisms
While these findings provide valuable insights, the underlying biological mechanisms driving the connection between a high degree of non-alcoholic fatty liver and NAFLD with the development of IBS remain the subject of ongoing research. However, several promising avenues have emerged.
One compelling theory suggests that the pathogenesis of NAFLD, characterized by liver fat accumulation and hepatic inflammation, may intersect with immune system activation and the development of IBS. Shared proinflammatory cytokines, such as TNF-α, IL-6, IL-8, and IL-1β, as well as reduced levels of IL-10, have been implicated in both NAFLD and IBS. These cytokines could play critical roles via Toll-like receptors (TLR), affecting peripheral and central nervous systems, gut motility, intestinal barrier integrity, and gut homeostasis.
Additionally, recent attention has focused on the intricate interplay between the gut and liver, known as the gut-liver axis. This axis involves the transport of bile salts and antimicrobial molecules from the liver to the intestinal lumen via the biliary tract and is crucial for maintaining gut eubiosis and preventing bacterial overgrowth. Diseased fatty liver may compromise this process, allowing harmful microbial by-products to accumulate, potentially exacerbating gut dysbiosis—a known factor in IBS pathogenesis.
Furthermore, the liver-brain-gut neural arc has emerged as a fascinating area of exploration. Research has demonstrated that hepatic vagal sensory afferent nerves may influence colonic regulatory T cells, impacting immune homeostasis and gut barrier function. Disruption of this neural arc could lead to intestinal disturbances and heightened susceptibility to IBS.
Gender Matters: A Female Predilection
Perhaps one of the most intriguing aspects of this research is the gender-specific nature of the association. While IBS predominantly affects females, the reasons behind this discrepancy have long remained a mystery. Recent data hint at the involvement of trace aminergic signaling and female reproductive hormones in the genesis of IBS. Disturbances in these systems could alter colonic ion secretion, immune reactivity, and serotonin levels, all factors implicated in IBS pathogenesis.
The observation that a positive association between non-alcoholic fatty liver and IBS risk was more pronounced in females opens new doors for research into the complex interplay of these factors.
Looking to the Future
In the ever-evolving landscape of medical research, connections between seemingly disparate conditions continue to emerge. The link between non-alcoholic fatty liver and IBS represents a fascinating area of exploration, with the potential to reshape our understanding of these conditions and inform future prevention and management strategies.
While this study has provided crucial insights, there is much work to be done. Future research will aim to elucidate the precise mechanisms driving this connection, explore gender-specific factors, and delve into the associations between NAFLD and different IBS subtypes.
In closing, the intricate relationship between non-alcoholic fatty liver and irritable bowel syndrome is a testament to the complexity of the human body and the boundless potential for discovery in the field of medical research.
FAQs:
What is Non-Alcoholic Fatty Liver Disease (NAFLD)?
Non-alcoholic fatty sedentary Liver Disease, or NAFLD, is a medical condition where fat accumulates in the liver of individuals who do not consume excessive alcohol. It is often associated with risk factors such as obesity, diabetes, and metabolic syndrome.
Is there a connection between IBS and NAFLD?
Emerging research suggests there may be a connection between IBS and NAFLD, as both conditions share common risk factors such as obesity and inflammation. Some studies have shown a higher prevalence of one condition in individuals with the other, but the exact nature of this connection is still being investigated.
How prevalent are IBS and NAFLD worldwide?
IBS affects millions of people worldwide, with estimates of prevalence varying by region. NAFLD, on the other hand, has a global prevalence of approximately 25% among adults.
What are the common symptoms of IBS?
Common symptoms of IBS include abdominal pain or discomfort, bloating, gas, and altered bowel habits, which can include diarrhea, constipation, or both.
What are the common symptoms of NAFLD?
In its early stages, NAFLD often presents with no noticeable symptoms. As it progresses, individuals may experience fatigue, abdominal discomfort, and, in advanced cases, symptoms of liver disease such as jaundice and abdominal swelling.
Are there any known risk factors for developing IBS?
Risk factors for IBS include a family history of the condition, infections that affect the gut, psychological stress, and certain dietary factors.
What are the risk factors associated with NAFLD?
Risk factors for NAFLD include obesity, type 2 diabetes, metabolic syndrome, high blood pressure, and high cholesterol. A sedentary lifestyle and poor dietary choices also contribute to the risk.
How is IBS typically diagnosed by healthcare professionals?
IBS is often diagnosed based on the patient's symptoms and the exclusion of other conditions with similar symptoms. Diagnostic criteria, such as the Rome criteria, are used to aid in diagnosis.
How is NAFLD diagnosed and confirmed?
The diagnosis of NAFLD typically involves blood tests, imaging studies like ultrasound or MRI, and sometimes a liver biopsy to confirm the presence and stage of the disease.
Can having IBS increase the risk of developing NAFLD?
While research suggests a correlation between IBS and NAFLD, it's important to note that having IBS alone does not necessarily increase the risk of developing NAFLD. Other factors, such as obesity and metabolic syndrome, are stronger predictors.
Can NAFLD lead to the development of IBS?
There is no direct evidence to suggest that NAFLD directly leads to the development of IBS. However, the shared risk factors and inflammatory processes may contribute to the co-occurrence of these conditions.
Is there a gender-specific association between IBS and NAFLD?
Some studies have suggested that the association between IBS and NAFLD may be more pronounced in females, but further research is needed to fully understand this gender-specific aspect.
What dietary changes can help manage both IBS and NAFLD?
Dietary modifications that can benefit both conditions include reducing the consumption of high-fat and high-sugar foods, increasing fiber intake, staying hydrated, and avoiding trigger foods that exacerbate IBS symptoms.
How does inflammation play a role in both conditions?
Inflammation is a key factor in both IBS and NAFLD. Chronic inflammation can contribute to the symptoms of IBS and the progression of liver damage in NAFLD.
What is the gut-liver axis, and how does it relate to IBS and NAFLD?
The gut-liver axis is a bidirectional communication system between the gut and the liver. Changes in gut microbiota and inflammation in the gut can impact liver function, potentially contributing to the development or progression of NAFLD.
Are there specific treatments or medications for individuals with both IBS and NAFLD?
Treatment for individuals with both conditions often involves a multidisciplinary approach, including dietary modifications, lifestyle changes, symptom management for IBS, and addressing risk factors for NAFLD.
How can lifestyle adjustments impact the management of IBS and NAFLD?
Lifestyle adjustments such as regular exercise, stress reduction techniques, and maintaining a healthy weight can positively impact both conditions by reducing symptoms and addressing underlying risk factors.
Can stress and mental health affect the severity of symptoms in both conditions?
Yes, stress, anxiety, and depression can exacerbate symptoms in both IBS and NAFLD. Managing mental health and stress is an important aspect of overall management.
What ongoing research is being conducted to further understand the relationship between IBS and NAFLD?
Ongoing research aims to elucidate the precise mechanisms connecting IBS and NAFLD, explore gender-specific factors, and identify potential interventions to manage both conditions effectively.
Video courtesy:
#115: Dr. Jill interviews Dr. Asia Muhammad tdiscuss the Gut axis and the epidemic of NAFLD
Jill Carnahan, MD
Image courtesy: MDPI (liver steatosis, Gut Liver axis
Related:
Menopausal Hormone Therapy and Non-Alcoholic Fatty Liver Disease: What's the Link? | Healthnewstrend
How Gut Microbes Use Taurine to Fight Off Pathogens | Healthnewstrend
Reference:
Non-alcoholic fatty liver is associated with increased risk of irritable bowel syndrome: a prospective cohort study | BMC Medicine | Full Text (biomedcentral.com)


