Muscle Weakness in Hypothyroidism: Symptoms, Causes & Treatment (Hypothyroid Myopathy)
Struggling with muscle weakness and low energy? Hypothyroidism, a common condition, could be behind it. Learn about Hypothyroid Myopathy (muscle weakness in hypothyroidism) - its causes, symptoms, and effective treatment options to regain strength and improve your quality of life. #hypothyroidism #muscleweakness #treatment
DR ANITA JAMWAL MS
3/30/20244 min read
According to a review in the National Centre for Biotechnology Information Up to 79% of people with hypothyroidism experience muscle weakness, cramps, stiffness, and fatigue (hypothyroid myopathy). This occurs because the body's underactive thyroid gland disrupts muscle metabolism. Early diagnosis through blood tests and physical exams is key. Treatment involves replacing the missing thyroid hormones with medication and physical therapy to regain muscle strength. With proper care, most patients see significant improvement within a year, although some residual weakness may linger. A team approach with doctors, nurses, therapists, and pharmacists ensures optimal patient outcomes.
Key Findings
Symptoms:
Muscle weakness, cramps, stiffness, and fatigue are the hallmarks of hypothyroid myopathy. Proximal muscles (shoulders, hips, thighs) are often most affected, causing difficulty with activities like climbing stairs or rising from a seated position.
Causes:
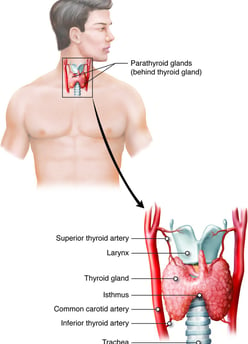
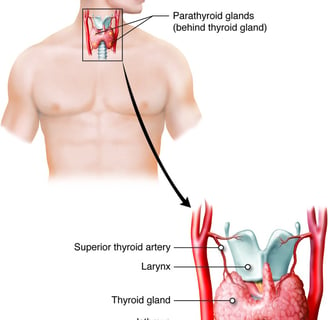
Hypothyroidism, a condition where the thyroid gland doesn't produce enough hormones, is the root cause of hypothyroid myopathy. Several factors can lead to hypothyroidism, including:
Autoimmune disorders (Hashimoto's thyroiditis)
Iodine deficiency
Thyroid surgery or radiation therapy
Medications
Congenital hypothyroidism
Aging
Pathophysiology:
The exact mechanism of muscle damage in hypothyroid myopathy is not fully understood. However, a lack of thyroid hormones disrupts cellular metabolism, impacting muscle function. This can lead to:
Reduced muscle fiber size and strength
Abnormal energy production within muscle cells
Accumulation of waste products in muscle tissue
Diagnosis:
Diagnosis involves a combination of clinical evaluation, blood tests, and sometimes electromyography or muscle biopsy.
Blood tests measure thyroid hormone levels (TSH, T4) and may show elevated creatine kinase (CK), a marker of muscle damage.
Physical examination assesses muscle strength, tone, and reflexes.
Electromyography may reveal abnormal electrical activity in muscles.
Muscle biopsy (rarely needed) can show structural changes in muscle tissue.
Treatment:
Treatment focuses on replacing missing thyroid hormones with levothyroxine medication. Early diagnosis and prompt treatment are essential for optimal recovery.
Levothyroxine dosage is individualized based on body weight, age, and underlying health conditions.
Regular monitoring of thyroid function ensures adequate hormone replacement.
Physical therapy can help improve muscle strength and function.
Prognosis:
With proper treatment, most patients with hypothyroid myopathy experience significant improvement in muscle strength and function within a year. However, recovery may take months and some residual weakness or fatigue may persist. Early diagnosis and intervention are crucial for a better prognosis.
Complications:
Untreated or severe hypothyroid myopathy can lead to complications like:
Increased risk of falls due to muscle weakness
Respiratory problems due to weakened breathing muscles
Cardiovascular issues
Prevention and Patient Education:
Patients with hypothyroidism should report any new or worsening muscle symptoms to their healthcare provider. Regular check-ups and adherence to treatment are essential.
Key Points:
Hypothyroid myopathy is a common consequence of hypothyroidism.
It presents with muscle weakness, cramps, stiffness, and fatigue.
Early diagnosis and treatment with levothyroxine are crucial for optimal outcomes.
An interprofessional team approach involving clinicians, nurses, therapists, and pharmacists optimizes patient care.
Regular monitoring and patient education are essential for successful management.
Hypothyroid myopathy is a prevalent condition affecting a significant portion of hypothyroid patients, leading to generalized muscle weakness and myalgias. The thyroid hormone plays a crucial role in metabolism and organ function, impacting the musculoskeletal system profoundly. This article delves into the various aspects of hypothyroid myopathy, including its symptoms, causes, evaluation, treatment, and prognosis.
Symptoms
Manifesting as generalized muscle weakness, cramps, stiffness, and fatigue, hypothyroid myopathy primarily affects proximal muscles such as those in the thighs, hips, shoulders, and neck. Activities like stair climbing, rising from a seated position, and lifting objects become challenging due to pronounced weakness in these muscle groups.
Etiology
Several factors contribute to the development of hypothyroid myopathy, including autoimmune disorders like Hashimoto thyroiditis, iodine deficiency, thyroid surgery or radiation therapy, certain medications, congenital hypothyroidism, and aging. These conditions lead to a deficiency of thyroid hormones, disrupting metabolic processes essential for muscle function.
Epidemiology
Hypothyroidism, predominantly observed in women, can manifest at any age, with a higher prevalence between 40 and 70 years. No specific racial predilection has been identified regarding this condition.
Pathophysiology
The pathogenesis of myopathy in hypothyroidism revolves around the significant influence of thyroid hormones on cellular metabolism. Thyroxine (T4) deficiency results in reduced mitochondrial oxidative capacity, abnormal glycogenolysis, and insulin resistance, leading to selective atrophy of type 2 muscle fibers. Muscle involvement is further characterized by changes in muscle fiber types, connective tissue deposition, and altered gene expression of skeletal muscle proteins.
History and Physical Examination
Clinical evaluation of hypothyroid myopathy involves assessing nonspecific symptoms such as myalgias, muscle cramps, fatigue, and progressive muscle weakness, particularly in proximal muscle groups. Physical examination reveals characteristic features like delayed muscle relaxation and, in some cases, muscle pseudohypertrophy.
Evaluation
Diagnosis of hypothyroid myopathy requires measuring thyroid-stimulating hormone (TSH) and T4 levels in the blood, along with assessing serum creatine kinase (CK) levels. Additional tests like electromyography (EMG) and muscle biopsy may aid in confirming the diagnosis.
Treatment / Management
Management primarily focuses on thyroid hormone replacement therapy, tailored according to the patient's body weight and response to treatment. Regular monitoring of thyroid function and CK levels is essential to track treatment efficacy and adjust medication dosage accordingly. Physical therapy complements medical treatment to improve muscle strength and function.
Prognosis
With appropriate treatment, the prognosis for hypothyroid myopathy is generally favorable, with most patients experiencing improvement in muscle strength and function. However, severe cases or delayed diagnosis may lead to permanent muscle damage and complications.
Complications
Complications of hypothyroid myopathy include muscle cramps, reduced mobility, increased risk of falls, and respiratory and cardiovascular complications. Prompt diagnosis and management are crucial in mitigating these risks.
Deterrence and Patient Education
Patients should be educated about the symptoms of hypothyroid myopathy and advised to report any worsening of muscle-related symptoms promptly. Regular follow-up appointments are essential to monitor thyroid function and adjust treatment as necessary.
Enhancing Healthcare Team Outcomes
Collaboration among healthcare professionals, including clinicians, nurses, pharmacists, and therapists, is vital in managing hypothyroid myopathy effectively. Regular communication, shared decision-making, and patient education contribute to improved patient outcomes and quality of life.
In conclusion, hypothyroid myopathy is a complex condition necessitating a comprehensive approach to diagnosis and management. By understanding its underlying mechanisms and implementing evidence-based interventions, healthcare teams can significantly improve patient outcomes and enhance overall quality of care.
Journal Reference
Fariduddin, M. M., & Bansal, N. (2023, November 18). Hypothyroid Myopathy. StatPearls - NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK519513/
Related
Disclaimer
The information on this website is for informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health care provider with any questions you may have regarding a medical condition or treatment. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
