Myocardial Insulin Resistance and Subclinical Atherosclerosis in Metabolic Syndrome Phenotypes
This study explores the link between impaired heart's ability to utilize insulin (cardiac insulin resistance) and the presence of both pre-diabetic markers (metabolic syndrome traits) and early signs of artery hardening (subclinical atherosclerosis) in individuals.
DR T S DIDWAL MD
3/20/20245 min read

This study, published in the journal Diabetes Care, explored the connection between heart metabolism and metabolic syndrome (MetS) in seemingly healthy individuals. MetS is a combination of factors like high blood pressure, elevated blood sugar, abnormal cholesterol, and excess belly fat, all of which increase the risk of heart disease, stroke, and type 2 diabetes. Researchers employed a sophisticated imaging technique called 18F-fluorodeoxyglucose positron emission tomography-magnetic resonance (18F-FDG PET-MR) to gauge myocardial FDG uptake, a marker reflecting heart metabolism. Their findings revealed that individuals with no myocardial FDG uptake had a significantly higher prevalence of MetS, hypertension, diabetes, and early signs of atherosclerosis when compared to those with higher myocardial FDG uptake.
Key Findings:
Individuals without detectable myocardial FDG uptake displayed a significantly higher prevalence of:
Metabolic syndrome (MetS)
High blood pressure (hypertension)
Diabetes
Early atherosclerosis (hardening of the arteries)
A higher insulin resistance index (HOMA-IR) is correlated with lower myocardial FDG uptake.
Participants with no myocardial FDG uptake at baseline who remained without it at follow-up had a higher chance of having MetS.
Participants who showed improvement in their cardiometabolic health between baseline and follow-up also demonstrated a significant increase in myocardial FDG uptake.
Three distinct cardiac metabolic profiles were observed in seemingly healthy individuals:
High Myocardial FDG Uptake: This phenotype is associated with a healthy cardiometabolic profile, a low prevalence of early atherosclerosis, and low bone marrow activation.
Intermediate Myocardial FDG Uptake: This phenotype is linked to an intermediate cardiometabolic profile and an intermediate prevalence of early atherosclerosis.
Low Myocardial FDG Uptake: This phenotype is associated with a poor cardiometabolic profile and a high prevalence of early atherosclerosis and bone marrow activation.
Limitations and Future Directions:
It's crucial to acknowledge that this study was observational and doesn't establish cause and effect. Further research is necessary to determine whether improving heart metabolism can help prevent or treat MetS and cardiovascular diseases.
Imagine your heart as a high-performance engine, and like any engine, it needs the right fuel to function optimally. A new study suggests that people with signs of an unhealthy heart metabolism, indicated by a reduced ability to utilize sugar for energy, are more likely to have metabolic syndrome (MetS), a cluster of conditions including high blood pressure, high blood sugar, unhealthy cholesterol levels, and excess belly fat. This condition significantly increases the risk of heart disease, stroke, and type 2 diabetes.
Traditionally, studying heart metabolism has been challenging. Most clinical studies involve strict pre-scan preparations that alter how the heart uses fuel, making it difficult to assess its natural metabolism. This new study, however, takes a different approach. Researchers employed a sophisticated imaging technique called 18F-fluorodeoxyglucose positron emission tomography-magnetic resonance (18F-FDG PET-MR) to gauge myocardial FDG uptake, a marker reflecting heart metabolism. Their findings revealed that individuals with no myocardial FDG uptake had a significantly higher prevalence of MetS, hypertension, diabetes, and early signs of atherosclerosis when compared to those with higher myocardial FDG uptake. Additionally, a stronger association emerged between higher insulin resistance (measured by HOMA-IR) and lower myocardial FDG uptake.
Investigating Hearts Under Normal Conditions
Researchers recruited a large group of middle-aged adults from the Progression of Early Subclinical Atherosclerosis (PESA) study. All participants were free of any known heart disease and underwent a special imaging technique called 18F-fluorodeoxyglucose positron emission tomography-magnetic resonance (18F-FDG PET-MR) to assess their myocardial (heart) FDG uptake. FDG is a type of sugar that the heart can use for energy, and the amount of FDG taken up by the heart reflects its metabolic activity.
Reduced sugar uptake is linked to an unhealthy profile.
The study revealed a fascinating connection: individuals with no detectable myocardial FDG uptake displayed a significantly higher prevalence of MetS, high blood pressure, diabetes, and early signs of atherosclerosis compared to those with higher myocardial FDG uptake. This suggests that a weakened ability of the heart to utilize sugar for energy might be associated with an unhealthy cardiometabolic profile.
Following Up: Metabolism and Risk Factors Change Together
The researchers followed the participants for nearly five years. Interestingly, those who lacked myocardial FDG uptake at the beginning and throughout the follow-up period were more likely to have MetS. Furthermore, participants who exhibited improvement in their overall cardiometabolic health between the two scans also showed a significant increase in myocardial FDG uptake. This two-way relationship between heart metabolism and cardiometabolic health strengthens the potential link between the two.
Three Metabolic Heart Profiles Emerge
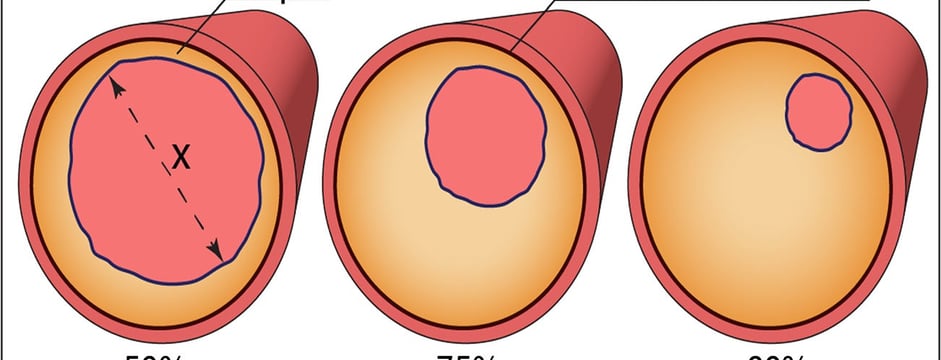
The study identified three distinct cardiac metabolic profiles based on myocardial FDG uptake levels:
High Uptake: This phenotype is associated with a healthy cardiometabolic profile, low prevalence of early atherosclerosis, and low bone marrow activation.
Intermediate Uptake: This phenotype is linked to an intermediate cardiometabolic profile and an intermediate prevalence of early atherosclerosis.
No Uptake: This phenotype is associated with a poor cardiometabolic profile, high prevalence of early atherosclerosis, and high bone marrow activation.
The study followed participants for nearly five years. Interestingly, those who lacked myocardial FDG uptake at the beginning and throughout the follow-up period were more likely to have MetS. Furthermore, participants who exhibited improvement in their overall cardiometabolic health between the two scans also showed a significant increase in myocardial FDG uptake.
Unraveling the Connection: A Cause-and-Effect Mystery
It's important to note that this study is observational and cannot determine cause and effect. More research is needed to understand whether improving heart metabolism can help prevent or treat MetS and cardiovascular diseases. However, these findings pave the way for exciting future investigations.
Future Directions: Can We Boost Heart Metabolism for Better Health?
Future studies could explore:
Whether interventions aimed at enhancing cardiac metabolism can improve MetS and cardiovascular health.
The underlying mechanisms link impaired heart metabolism to MetS and cardiovascular disease development.
The potential of using myocardial FDG uptake as a tool to identify individuals at high risk of MetS and cardiovascular diseases.
By delving deeper into this association, researchers may uncover new avenues for preventing and managing MetS and cardiovascular diseases, potentially leading to the development of strategies to keep our hearts healthy and metabolically flexible.
To Summarize
This study investigated the link between heart health and metabolism in seemingly healthy people.
People with poor heart metabolism, measured by how well the heart uses sugar for energy, were more likely to have metabolic syndrome.
Metabolic syndrome is a group of conditions that raise the risk of heart disease, stroke, and diabetes.
The study suggests that a poorly functioning heart and metabolic syndrome might be connected.
More research is needed to see if improving heart metabolism can help prevent or treat metabolic syndrome and heart disease.
Journal Reference
Devesa, A., Fuster, V., Vazirani, R., García-Lunar, I., Oliva, B., España, S., Moreno-Arciniegas, A., Sanz, J., Perez-Herreras, C., Bueno, H., Lara-Pezzi, E., García-Alvarez, A., de Vega, V. M., Fernández-Friera, L., Trivieri, M. G., Fernández-Ortiz, A., Rossello, X., Sanchez-Gonzalez, J., & Ibanez, B. (2023). Cardiac Insulin Resistance in Subjects With Metabolic Syndrome Traits and Early Subclinical Atherosclerosis. Diabetes care, 46(11), 2050–2057. https://doi.org/10.2337/dc23-0871
Related
Understanding Metabolic Syndrome: A Rising Global Health Concern
Medical disclaimer
The information on this website is for educational and informational purposes only, and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition or treatment, and before undertaking a new healthcare regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
