NAFLD: How Fatty Liver Disease Impacts Heart Health
Discover the surprising connection between nonalcoholic fatty liver disease (NAFLD) and atherosclerosis. Learn how these conditions are linked by inflammation and immune system responses, and explore strategies for prevention and management.
DR T S DIDWAL MD (Internal Medicine)
10/23/20248 min read

The connection between nonalcoholic fatty liver disease (NAFLD) and atherosclerosis is more significant than previously thought. According to research published in Medicine, both conditions share similar inflammatory pathways, triggered by elevated levels of a protein called Matrix Metalloproteinase 9 (MMP9). This research suggests that early detection and prevention of both conditions are crucial. Addressing both liver and heart health together through lifestyle modifications and potentially future-targeted treatments is key. Understanding this connection emphasizes the importance of a holistic approach to healthcare.
Key points
NAFLD and Atherosclerosis Connection: The article highlights a strong link between nonalcoholic fatty liver disease (NAFLD) and atherosclerosis.
Shared Inflammatory Pathways: Both conditions involve similar inflammatory mechanisms, particularly involving MMP9.
Immune System Role: The immune system plays a crucial role in both conditions, with macrophages and other immune cells contributing to inflammation.
Early Detection and Prevention: Early detection is crucial for both conditions, as they can often coexist. Prevention strategies, such as healthy lifestyle choices, are essential.
Treatment Implications: Future treatments might focus on addressing both conditions simultaneously, targeting shared mechanisms.
MMP9 as a Key Player: MMP9, a protein involved in inflammation, is a potential marker and target for future therapies.
Holistic Approach to Health: The research emphasizes the importance of a holistic approach to healthcare, considering the interconnectedness of different bodily systems.
The Hidden Connection: Understanding the Link Between Fatty Liver Disease and Heart Health
Most people don't think about their liver when considering heart health, but groundbreaking research suggests these two body systems are more closely connected than we previously thought. A fascinating new study has revealed important insights into how nonalcoholic fatty liver disease (NAFLD) and atherosclerosis—the buildup of plaque in our arteries—may be working together to impact our health in surprising ways.
Understanding the Key Players
Before we dive into the connection, let's break down these two conditions:
Nonalcoholic Fatty Liver Disease (NAFLD) is the most common liver disease worldwide, affecting millions of people. As the name suggests, it occurs when excess fat builds up in the liver of people who drink little to no alcohol. Think of it as your liver becoming "marbled" like a fatty steak.
Atherosclerosis is essentially the hardening and narrowing of your arteries due to plaque buildup. Imagine your arteries as highways, and atherosclerosis as a gradual accumulation of debris that narrows these crucial pathways, making it harder for blood to flow freely.
The Surprising Connection
For years, doctors have noticed that patients with fatty liver disease often develop heart problems, and vice versa. But understanding exactly why this happens has been like trying to solve a complex puzzle. Recent research has unveiled some fascinating pieces of this puzzle, suggesting that these conditions don't just occur together by chance—they're actively working together to affect our health.
The Common Thread: Inflammation
At the heart of this connection lies inflammation—our body's response to injury or stress. The research reveals that both conditions share similar inflammatory pathways, almost like they're speaking the same language of dysfunction. One particular protein, called Matrix Metalloproteinase 9 (MMP9), appears to play a starring role in this story.
Think of MMP9 as a molecular messenger that's unusually active in both conditions. When scientists looked at tissue samples from patients with both NAFLD and atherosclerosis, they found elevated levels of this protein, suggesting it might be a key player in coordinating the development of both diseases.
The Immune System Connection
Our immune system, usually our faithful defender against illness, appears to be deeply involved in this relationship. The research shows that both conditions trigger similar immune responses, almost like a domino effect where one condition can amplify the other.
This immune response involves several key players:
Specialized immune cells called macrophages
Various inflammatory signaling molecules
Complex protein networks that coordinate immune responses
Why This Matters for Your Health
This research isn't just academic – it has real implications for how we might prevent and treat these conditions in the future. Understanding that NAFLD and atherosclerosis are linked means that:
Early Detection is Crucial: If you're diagnosed with one condition, your healthcare provider should be vigilant about monitoring for the other.
Treatment Approaches Might Change: future treatments might target both conditions simultaneously, potentially offering more effective results.
Prevention Strategies Could Be More Effective: Understanding the shared mechanisms means we might be able to prevent both conditions through similar lifestyle modifications.
Understanding the Role of MMP9 and Genetics
In both NAFLD and atherosclerosis, a protein called Matrix Metalloproteinase 9 (MMP9) is involved in inflammation. Think of MMP9 as a messenger that signals the body to create inflammation. In people with both liver disease and heart disease, this protein is often found at higher levels, which means it could be a clue for doctors to detect and treat these conditions early.
As for genetics, certain inherited traits might make some people more likely to develop both NAFLD and heart disease. For example, specific genes that affect how the body processes fat could increase the risk of both conditions. While we can’t change our genes, understanding their role helps doctors create more personalized treatment plans.
More Scientific Research on the association of fatty liver disease (MAFLD) and atherosclerotic cardiovascular disease (ASCVD)
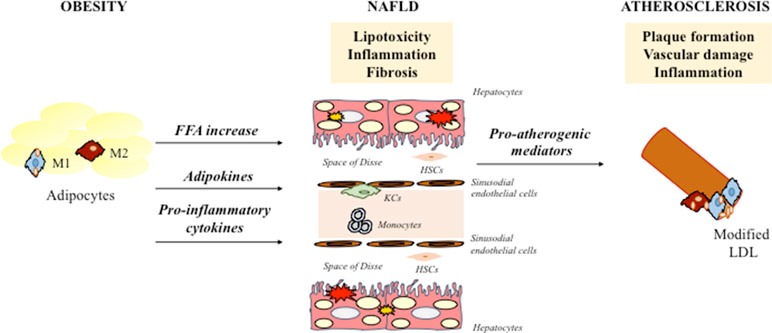
The relationship between metabolic dysfunction-associated fatty liver disease (MAFLD) and atherosclerotic cardiovascular disease (ASCVD) has been extensively studied. MAFLD is closely related to ASCVD, with recent studies showing that MAFLD is significantly associated with ASCVD risk. According to new research in The American Journal of the Medical Sciences, this association is likely due to shared risk factors such as insulin resistance (IR), obesity, and inflammation.
Several mechanisms may link MAFLD to ASCVD. Abnormal fat metabolism in MAFLD can lead to dyslipidemia, which is a risk factor for atherosclerosis. Adipokine disorders, particularly low adiponectin levels, can also contribute to ASCVD risk. Obesity, a common comorbidity with MAFLD, is associated with both liver and heart disease. IR, a key feature of MAFLD, can lead to dyslipidemia, inflammation, and endothelial dysfunction. Finally, inflammation plays a crucial role in both MAFLD and ASCVD, with increased levels of inflammatory markers associated with higher risk of cardiovascular events.
Genetic factors may also contribute to the association between MAFLD and ASCVD. Studies have identified several genetic variants associated with MAFLD, some of which may also influence ASCVD risk. For example, the PNPLA3 rs738409 G allele has been associated with a lower risk of CHD in MAFLD patients, possibly due to its effects on lipid metabolism.
Looking Ahead: What This Means for Future Treatment
This research opens up several exciting possibilities for future treatments:
Short-term Implications
Better screening protocols for patients with either condition
More comprehensive treatment approaches that consider both liver and heart health
Improved risk assessment for patients
Long-term Possibilities
Development of new drugs targeting shared disease mechanisms
More personalized treatment approaches based on individual inflammatory profiles
Better prevention strategies that address both conditions simultaneously
Practical Steps for Protecting Your Liver and Heart Health
While this research progresses, there are several evidence-based steps you can take to protect both your liver and heart health:
1. Maintain a Healthy Diet
Focus on whole foods
Limit processed foods and added sugars
Include plenty of fruits, vegetables, and lean proteins
2. Stay Active
Regular exercise benefits both your liver and heart
Aim for at least 150 minutes of moderate activity per week
Include both cardio and strength training
3. Monitor Your Health
Regular check-ups with your healthcare provider
Keep track of key health markers like blood pressure and cholesterol
Be aware of family history for both conditions
The Bigger Picture
This research represents a significant step forward in understanding how different systems in our body interact and influence each other. It's a reminder that our body works as an interconnected whole, not as isolated systems.
The discovery of shared mechanisms between NAFLD and atherosclerosis highlights the importance of taking a holistic approach to health. It's not just about treating individual conditions; it's about understanding how they relate to each other and addressing the root causes that might be affecting multiple systems in our bodies.
Conclusion
The connection between fatty liver disease and atherosclerosis is a perfect example of how medical research continues to reveal new insights about how our bodies work. By understanding these connections, we're better equipped to prevent and treat these conditions effectively.
As research continues, we can expect to see more integrated approaches to treating these conditions, potentially leading to better outcomes for patients affected by either or both diseases. In the meantime, maintaining a healthy lifestyle remains our best defense against both conditions.
FAQs on the Connection Between NAFLD and Atherosclerosis
1. What is the relationship between NAFLD and atherosclerosis?
NAFLD and atherosclerosis are closely linked conditions, sharing similar inflammatory mechanisms and often coexisting in patients.
2. How does inflammation contribute to both conditions?
Elevated levels of MMP9, a protein involved in inflammation, are associated with both NAFLD and atherosclerosis. This suggests that inflammation plays a central role in the development of both conditions.
3. What are the early signs and symptoms of NAFLD and atherosclerosis?
NAFLD often has no symptoms in the early stages. As it progresses, symptoms may include fatigue, abdominal pain, weight loss, and jaundice. Atherosclerosis can lead to symptoms like chest pain, shortness of breath, and heart attack.
4. Can lifestyle changes help prevent or manage these conditions?
Yes, lifestyle changes are crucial for preventing and managing both NAFLD and atherosclerosis. These include maintaining a healthy diet, regular exercise, weight management, and avoiding excessive alcohol consumption.
5. Are there specific treatments available for NAFLD and atherosclerosis?
While there's no cure for NAFLD or atherosclerosis, treatments may focus on managing symptoms, addressing underlying risk factors, and preventing complications. Medications and procedures may be used in certain cases.
6. Can NAFLD lead to heart disease?
Yes, NAFLD is a risk factor for heart disease. The connection between the two conditions is due to shared inflammatory processes and the increased risk of cardiovascular events.
7. How often should I get screened for NAFLD and atherosclerosis?
If you have risk factors for either condition, such as obesity, diabetes, or high blood pressure, regular screenings are recommended. Consult with your healthcare provider for personalized screening guidelines.
8. Is it possible to reverse NAFLD or atherosclerosis?
While complete reversal may be challenging, lifestyle changes and early intervention can often improve liver health and reduce the progression of atherosclerosis.
9. What role does genetics play in these conditions?
Genetics can contribute to the risk of developing NAFLD and atherosclerosis. However, lifestyle factors also play a significant role.
10. Can stress affect NAFLD and atherosclerosis?
Chronic stress has been linked to both NAFLD and atherosclerosis. Managing stress through techniques like relaxation exercises and mindfulness can be beneficial.
Related Articles
Thyromimetics: A New Frontier in Liver Disease Treatment
MASLD and cardiovascular disease:How Fatty Liver Can Harm Your Heart?
Myocardial Insulin Resistance and Subclinical Atherosclerosis in Metabolic Syndrome Phenotypes
CardioRACE Study: Unveiling the Winning Exercise Strategy Against Heart Disease in Overweight Adults
Journal References
Wen, W., Fan, H., Zhang, S., Hu, S., Chen, C., Tang, J., You, Y., Wang, C., Li, J., Luo, L., Cheng, Y., Zhou, M., Zhao, X., Tan, T., Xu, F., Fu, X., Chen, J., Dong, P., Zhang, X., Wang, M., … Feng, Y. (2024). Associations between metabolic dysfunction-associated fatty liver disease and atherosclerotic cardiovascular disease. The American journal of the medical sciences, S0002-9629(24)01323-5. Advance online publication. https://doi.org/10.1016/j.amjms.2024.06.022
Lv, Q., Han, Q., Wen, Z., Pan, Y., & Chen, J. (2024, January 5). The association between atherosclerosis and nonalcoholic fatty liver disease. Medicine, 103(1), e36815. https://doi.org/10.1097/md.0000000000036815
Image credit: https://www.frontiersin.org/files/Articles/452744/fphar-10-00604-HTML/image_m/fphar-10-00604-g001.jpg
Medical disclaimer
The information on this website is for educational and informational purposes only, and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition or treatment, and before undertaking a new healthcare regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
About the Author:
Dr.T.S. Didwal, MD, is an experienced Internal Medicine Physician with over 30 years of practice. Specializing in internal medicine, he is dedicated to promoting wellness, preventive health, and fitness as core components of patient care. Dr. Didwal’s approach emphasizes the importance of proactive health management, encouraging patients to adopt healthy lifestyles, focus on fitness, and prioritize preventive measures. His expertise includes early detection and treatment of diseases, with a particular focus on preventing chronic conditions before they develop. Through personalized care, he helps patients understand the importance of regular health screenings, proper nutrition, exercise, and stress management in maintaining overall well-being.
With a commitment to improving patient outcomes, Dr. Didwal integrates the latest medical advancements with a compassionate approach. He believes in empowering patients to take control of their health and make informed decisions that support long-term wellness.
