Nanotherapy: A New Hope for Heart Disease
Discover how nanotechnology is revolutionizing heart disease treatment. Learn about the groundbreaking "Trojan horse" nanoparticle therapy that could potentially cure atherosclerosis and offer new hope for millions of people at risk of heart attacks and strokes.
DR T S DIDWAL MD (Internal Medicine)
10/22/20247 min read
"Trojan horse" nanoparticle therapy is a promising new approach to treating atherosclerosis, the underlying cause of heart attacks and strokes. According to research published in Nature Communications, these nanoparticles target and treat problematic areas in blood vessels without affecting healthy tissues. They carry a chemical inhibitor that reactivates the body's natural cleanup process, which is often impaired in atherosclerosis. This therapy has shown success in both mice and pigs, and it has the potential to revolutionize cardiovascular medicine. However, further research and clinical trials are needed before it becomes available to patients.
Key points
Targeted treatment: The nanoparticles specifically target inflammatory cells within atherosclerotic plaques, reducing the risk of side effects.
Reactivation of natural cleanup process: The therapy helps restore the body's ability to clear away dead and dying cells within plaques.
Promising results in animal studies: The therapy has shown effectiveness in both mice and pigs.
Potential for revolutionizing cardiovascular medicine: This approach could offer a new way to treat atherosclerosis and potentially other inflammatory diseases.
Ongoing development: Further research and clinical trials are needed before the therapy becomes available to patients.
The Next Generation of Heart Disease Treatment: How 'Trojan Horse' Nanoparticles Could Revolutionize Cardiovascular Medicine
Cardiovascular disease remains the leading cause of death in the United States, despite decades of medical advances. While we've made significant strides in managing risk factors like high blood pressure and cholesterol, heart disease continues to pose a major public health challenge. However, exciting new research in nanomedicine might change this landscape dramatically, offering a more targeted and potentially safer approach to treating atherosclerosis, the underlying cause of most heart attacks and strokes.
Understanding the Enemy: Atherosclerosis
Before diving into the breakthrough, let's understand what we're fighting. Atherosclerosis is fundamentally an inflammatory disorder where fatty deposits build up in your arteries. Think of it like a slow-moving traffic jam in your blood vessels. As these buildups (called plaques) grow, they can eventually rupture, potentially triggering a heart attack or stroke.
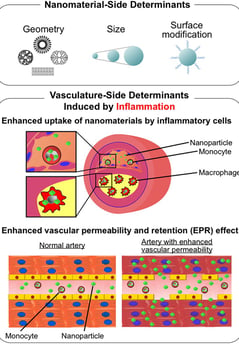
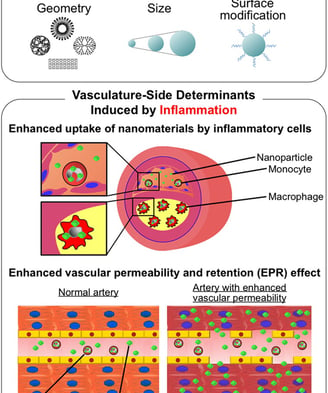
One of the key problems in atherosclerosis is the body's inability to clear away dead and dying cells within these plaques. In a healthy body, specialized immune cells called macrophages act like cellular garbage collectors, engulfing and removing dead cells through a process known as efferocytosis. However, in atherosclerosis, this cleanup system breaks down, leading to a growing collection of cellular debris that makes the plaques more unstable and dangerous.
The CD47 Discovery: A Double-Edged Sword
Scientists previously discovered that many of these troublesome cells display a protein called CD47 on their surface—essentially a "don't eat me" signal that prevents macrophages from clearing them away. Initial treatments targeting CD47 with antibodies showed promise in reducing plaque buildup, but there was a significant catch: these antibodies also caused the removal of healthy red blood cells, leading to anemia. This side effect made the treatment impractical for many heart disease patients who couldn't afford to have their oxygen-carrying capacity reduced.
Enter the 'Trojan Horse' Nanoparticle
This is where the latest breakthrough comes in. Researchers have developed what they're calling a "Trojan horse" nanotherapy—microscopic particles that specifically target and treat problematic areas in blood vessels without affecting healthy tissues. These nanoparticles, made from single-walled carbon nanotubes (SWNTs), are designed to be preferentially taken up by inflammatory immune cells within atherosclerotic plaques.
The genius of this approach lies in its precision. Instead of flooding the entire body with medication, these nanoparticles deliver their therapeutic payload specifically to the cells that need it most. They carry a chemical inhibitor that blocks SHP-1, a protein downstream of the CD47 pathway, effectively reactivating the natural cleanup process without causing system-wide side effects.
From Mice to Pigs: Scaling Up Success
While many promising treatments work well in mice but fail in larger animals, this nanotherapy has now shown success in pigs—a crucial stepping stone toward human trials. Pigs are particularly good models for human heart disease because their cardiovascular system is remarkably similar to ours in size and function.
The research team successfully scaled up the production of these nanoparticles to quantities that would be needed for human treatment—more than 1,000 times the amount needed for mouse studies. More importantly, this scaled-up version maintained its effectiveness and safety profile. When tested in pigs with early-stage atherosclerosis, the treatment:
Reduced inflammation in arterial plaques
decreased the accumulation of dead cells
Didn't cause anemia or other significant side effects
Specifically targeted inflammatory cells within plaques
The Science Behind the Success
The treatment's effectiveness appears to work through multiple mechanisms. Beyond simply helping clear away cellular debris, the therapy triggers beneficial changes in gene expression within the blood vessel wall. One particularly interesting finding was the upregulation of HMOX1, an enzyme known to protect against atherosclerosis by helping break down potentially harmful heme compounds and reducing inflammation.
Other activated genes were found to help with:
Phagosome maturation (the cellular structures where debris is processed)
Cell migration
Anti-inflammatory responses
Immune system regulation
Looking Ahead: Promise and Caution
While these results are exciting, it's important to note that this research is still in its early stages. The current studies only looked at early-stage plaques, and longer-term studies with more advanced disease are needed. Additionally, while no major safety concerns were identified, careful monitoring will be necessary as the technology moves toward human trials.
Why This Matters: The Bigger Picture
This research represents more than just another potential treatment for heart disease. It showcases a new paradigm in medicine: highly targeted therapies that can affect specific cellular processes in particular locations while leaving healthy tissues undisturbed. This approach could potentially revolutionize how we treat not just heart disease, but a wide range of conditions where inflammation plays a key role.
The technology also demonstrates the power of interdisciplinary science. This breakthrough combines advances in:
Nanotechnology
Immunology
Cardiovascular medicine
Drug delivery systems
Molecular biology
The Road to Clinical Use
Before this treatment becomes available to patients, several hurdles need to be cleared:
Longer-term studies in animals with more advanced disease
Further safety testing to understand any potential risks
Clinical trials in humans
Manufacturing scale-up for commercial production
However, the successful transition from mouse studies to pig models, while maintaining effectiveness and safety, is a significant milestone that suggests this technology has real potential for human use.
A New Hope for Heart Disease Treatment
As our understanding of cardiovascular disease has evolved, it's become clear that we need more sophisticated approaches than simply lowering cholesterol or blood pressure. This nanotherapy represents a new generation of treatments that work with the body's natural processes to address the root causes of atherosclerosis.
The ability to selectively target diseased tissue while sparing healthy cells could be a game-changer in cardiovascular medicine. If successful in humans, this approach could offer new hope to millions of people at risk for heart attacks and strokes, potentially reducing the massive public health burden of cardiovascular disease.
While we must remain cautiously optimistic as this technology continues through the development pipeline, the principles demonstrated here—precise targeting, selective drug delivery, and working with natural cellular processes—likely represent the future of medicine. As we continue to understand more about the complex interplay between inflammation, immunity, and cardiovascular disease, treatments like this "Trojan horse" nanotherapy may become powerful tools in our medical arsenal.
Remember, while this research is promising, it's still in development. If you're concerned about heart disease, the best course of action remains working with your healthcare provider to manage traditional risk factors through proven methods like maintaining a healthy diet, regular exercise, and appropriate medical therapy when needed.
The journey from laboratory breakthrough to bedside treatment is long and complex, but each step forward brings us closer to better solutions for one of humanity's most persistent health challenges. This nanotherapy approach represents not just a potential new treatment but a new way of thinking about how we can combat disease at the cellular level with unprecedented precision.
FAQs
1. What is atherosclerosis? Atherosclerosis is a disease where fatty deposits build up in the arteries, leading to a narrowing of the blood vessels and potentially causing heart attacks or strokes.
2. How does the "Trojan horse" nanotherapy work? These nanoparticles are designed to target and treat inflammatory cells within atherosclerotic plaques. They deliver a therapeutic payload that reactivates the body's natural cleanup process without causing system-wide side effects.
3. Why is this therapy called a "Trojan horse"? The nanoparticles are likened to a Trojan horse because they are designed to be taken up by harmful cells within the plaques, allowing them to deliver their therapeutic payload directly to the problem area.
4. Has this therapy been tested in humans yet? No, this therapy is still in the early stages of development and has only been tested in animals.
5. What are the potential side effects of this therapy? While no major safety concerns have been identified in animal studies, further research is needed to fully understand any potential risks.
6. How long will it take for this therapy to become available to patients? The development process can be lengthy, and it may take several years for this therapy to become available to patients.
7. Is this therapy the only potential treatment for atherosclerosis? While this therapy shows promise, it is not the only potential treatment for atherosclerosis. Other approaches, such as lifestyle changes, medications, and surgical interventions, are also available.
8. Will this therapy be effective for all stages of atherosclerosis? The current studies have focused on early-stage atherosclerosis. More research is needed to determine the effectiveness of this therapy for more advanced stages of the disease.
9. Could this therapy be used to treat other diseases besides atherosclerosis? The principles behind this therapy could potentially be applied to other diseases where inflammation plays a key role, such as arthritis and Alzheimer's disease.
Related Article
Small Dense LDL: A Risk Factor for Coronary Artery Calcification
Journal Reference
Bamezai, S., Zhang, Y., Kumari, M. et al. Pro-efferocytic nanotherapies reduce vascular inflammation without inducing anemia in a large animal model of atherosclerosis. Nat Commun 15, 8034 (2024). https://doi.org/10.1038/s41467-024-52005-1
Image credit :https://www.frontiersin.org/files/Articles/312764/fcvm-04-00087-HTML/image_m/fcvm-04-00087-g001.jpg
Disclaimer
The information on this website is for informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition or treatment. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
About the Author:
Dr. T.S. Didwal, MD, is an experienced Internal Medicine Physician with over 30 years of clinical practice. Specializing in internal medicine, he is dedicated to promoting wellness, preventive health, and fitness as core components of patient care. Dr. Didwal’s approach emphasizes the importance of proactive health management, encouraging patients to adopt healthy lifestyles, focus on fitness, and prioritize preventive measures. His expertise includes early detection and treatment of diseases, with a particular focus on preventing chronic conditions before they develop. Through personalized care, he helps patients understand the importance of regular health screenings, proper nutrition, exercise, and stress management in maintaining overall well-being.
With a commitment to improving patient outcomes, Dr. Didwal integrates the latest medical advancements with a compassionate approach. He believes in empowering patients to take control of their health and make informed decisions that support long-term wellness.
