Osteopenia and Fall Prevention: Effective Strategies for Older Adults
Discover effective strategies to prevent falls in older adults with osteopenia. Learn about lifestyle modifications, home safety tips, and medical interventions to reduce the risk of fractures and improve overall quality of life.
DR T S DIDWAL MD
9/30/20249 min read
According to a review published in The Lancet Diabetes & Endocrinology. Osteopenia, a condition characterized by low bone density, is prevalent among older adults and significantly increases the risk of fractures. While it's often considered a precursor to osteoporosis, osteopenia itself can lead to fractures due to its prevalence. Effective management of osteopenia involves a combination of lifestyle modifications, fall prevention strategies, and pharmacological interventions. By understanding the factors influencing fracture risk, individuals with osteopenia can make informed decisions about their care and reduce the likelihood of fractures. However, the management of osteopenia remains a complex issue with ongoing debates and challenges, highlighting the need for further research and development in this area.
Key points
Osteopenia Definition: Osteopenia is a bone mineral density (BMD) T-score between -1.0 and -2.5, indicating a bone density lower than normal but not yet osteoporosis.
Fracture Risk: While osteopenia carries a lower fracture risk than osteoporosis, the high prevalence of osteopenia means that most fractures in older adults occur in this group.
Risk Factors: Factors influencing fracture risk include BMD, age, fracture history, nationality, ethnicity, and lifestyle factors like smoking and alcohol consumption.
Diagnosis and Assessment: Osteopenia diagnosis involves a bone density scan, and fracture risk should be assessed using tools like FRAX®.
Management Strategies: Management strategies include lifestyle modifications (exercise, diet), fall prevention, and pharmacological interventions like bisphosphonates.
Personalized Approach: Osteopenia management should be tailored to individual risk profiles, considering factors like age, fracture risk, and treatment preferences.
Challenges and Future Directions: Challenges in osteopenia management include overdiagnosis, long-term safety of bisphosphonates, treatment in younger women, and male osteopenia. Future research areas include improved risk assessment, novel treatments, and personalized management strategies.
Osteopenia Management in Older Adults: A Comprehensive Guide
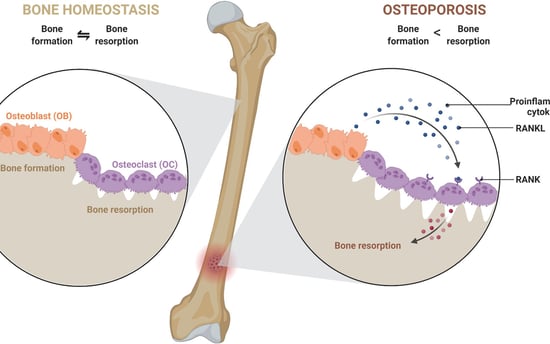
As our population ages, bone health becomes an increasingly important aspect of overall well-being. You may have heard of osteoporosis, a condition characterized by low bone mass and increased fracture risk. But what about its lesser-known cousin, osteopenia? In this comprehensive guide, we'll explore osteopenia, its significance in older adults, and the latest evidence-based approaches to its management.
What is osteopenia?
Osteopenia is a term that has evolved over time. Originally, it was a qualitative description used by radiologists to describe bones that appeared less dense on X-rays. However, since 1994, osteopenia has taken on a more precise, quantitative meaning in the medical community.
Definition
Today, osteopenia is defined as a bone mineral density (BMD) T-score between -1.0 and -2.5. This score is derived from a bone density scan, typically a DEXA (Dual-Energy X-ray Absorptiometry) scan, which compares an individual's bone density to that of a healthy young adult.
To put this in perspective:
A T-score above -1.0 is considered normal bone density.
A T-score between -1.0 and -2.5 indicates osteopenia.
A T-score of -2.5 or lower signifies osteoporosis.
Prevalence in Older Adults
Osteopenia is surprisingly common, especially among older women. More than 60% of White women over the age of 64 have osteopenia. This high prevalence makes osteopenia a significant public health concern, particularly given its association with increased fracture risk.
Understanding Fracture Risk in Osteopenia
While the fracture risk for individuals with osteopenia is generally lower than for those with osteoporosis, the sheer number of people with osteopenia means that most fractures actually occur in this group. This counterintuitive fact underscores the importance of addressing osteopenia in our aging population.
Factors Influencing Fracture Risk
Fracture risk in osteopenia isn't uniform. It can vary widely based on several factors:
Bone Mineral Density (BMD): Even within the osteopenic range, lower BMD scores are associated with higher fracture risk.
Age: As we age, fracture risk increases independently of BMD.
Fracture History: Previous fractures, especially recent ones, significantly increase the risk of future fractures.
Nationality and Ethnicity: Fracture risk varies across different populations, influenced by genetic and environmental factors.
Other Risk Factors: Family history of fractures, low body weight, smoking, excessive alcohol consumption, and certain medications can all contribute to increased fracture risk.
Diagnosis and Risk Assessment
Given the variability in fracture risk among osteopenic individuals, a diagnosis of osteopenia alone is neither an indication for immediate intervention nor a reason for complacency. Instead, it should prompt a more comprehensive assessment of fracture risk.
Fracture Risk Calculation
Bone mineral density should be incorporated into a quantitative fracture risk calculation. Tools like the FRAX® (Fracture Risk Assessment Tool) developed by the World Health Organization can be invaluable in this process. These tools consider multiple risk factors to provide a more accurate estimate of an individual's 10-year probability of major osteoporotic fracture.
Management Strategies for Osteopenia
The management of osteopenia in older adults should be tailored to the individual's specific risk profile. Here are some key strategies:
Lifestyle Modifications
Regardless of fracture risk, all individuals with osteopenia can benefit from lifestyle changes that promote bone health:
Regular Weight-Bearing Exercise: Activities like walking, jogging, or dancing can help maintain and even improve bone density.
Balanced Diet: Ensuring adequate calcium and vitamin D intake is crucial for bone health.
Smoking Cessation: Smoking is detrimental to bone health and should be avoided.
Limiting alcohol consumption: Excessive alcohol intake can negatively impact bone density.
Fall Prevention
Since fractures often result from falls, implementing fall prevention strategies is crucial:
Home Safety Assessment: Removing tripping hazards and improving lighting can reduce fall risk.
Balance Training: Exercises that improve balance and coordination can help prevent falls.
Medication Review: Some medications can increase fall risk and may need to be adjusted.
Pharmacological Interventions
For individuals at higher risk of fracture, medication may be recommended. The most commonly used and studied medications for osteopenia are bisphosphonates.
Evidence for Bisphosphonate Use
Recent evidence from clinical trials has shown that both oral and intravenous bisphosphonates can cost-effectively reduce fractures in older women with osteopenia. This is a significant development, as it provides a clear treatment option for those at higher risk.
When to Consider Treatment
The decision to start pharmacological treatment should be based on a comprehensive assessment of fracture risk. Current evidence suggests that for patients over 65 years old who are motivated to receive treatment, a 10-year major osteoporotic fracture risk of 10-15% could be an acceptable indication for treatment with generic bisphosphonates.
Personalized Approach to Osteopenia Management
Given the variability in fracture risk and the potential benefits and risks of treatment, a personalized approach to osteopenia management is crucial. Here's a step-by-step guide to developing a management plan:
Assess Bone Mineral Density: Start with a bone density scan to determine if the patient falls in the osteopenic range.
Calculate Fracture Risk: Use a tool like FRAX® to estimate the 10-year probability of major osteoporotic fracture, incorporating BMD and other risk factors.
Discuss Risk and Treatment Options: Engage in a thorough discussion with the patient about their fracture risk and the potential benefits and risks of various management strategies.
Implement Lifestyle Modifications: Encourage all patients to adopt bone-healthy lifestyle habits, regardless of their fracture risk.
Consider Pharmacological Treatment: For patients with higher fracture risk (10-15% 10-year risk of major osteoporotic fracture) who are over 65 and motivated to receive treatment, consider initiating bisphosphonate therapy.
Monitor and Reassess: Regularly monitor the patient's bone health and reassess fracture risk over time. Treatment plans may need to be adjusted based on changes in risk factors or response to interventions.
Challenges and controversies in Osteopenia Management
While recent evidence has provided clearer guidance on osteopenia management, some challenges and controversies remain:
Overdiagnosis and Overtreatment
There's an ongoing debate about the potential for overdiagnosis and overtreatment of osteopenia. Critics argue that labeling a large portion of the older population with a "pre-disease" state could lead to unnecessary anxiety and treatment.
Long-Term Safety of Bisphosphonates
While bisphosphonates have shown efficacy in reducing fracture risk, concerns about long-term safety, including rare but serious side effects like atypical femur fractures and osteonecrosis of the jaw, have led to debates about the optimal duration of treatment.
Treatment in Younger Postmenopausal Women
Most studies on osteopenia treatment have focused on older women. The benefits and risks of pharmacological interventions in younger postmenopausal women with osteopenia are less clear and require further research.
Male Osteopenia
While osteopenia is more common in women, it also affects men. However, most studies have focused on women, leaving some uncertainty about the optimal management strategies for men with osteopenia.
Future Directions in Osteopenia Research and Management
As our understanding of osteopenia evolves, several areas of research and development hold promise for improving its management:
1. Improved Risk Assessment Tools: Refining fracture risk assessment tools to provide more accurate and personalized risk estimates.
2. Novel Pharmacological Interventions: Developing new medications that can effectively reduce fracture risk with improved safety profiles.
3. Personalized Treatment Algorithms: Creating more sophisticated algorithms that can guide treatment decisions based on individual patient characteristics and preferences.
4. Long-Term Studies: Conducting longer-term studies to better understand the long-term benefits and risks of various management strategies.
5. Focus on Prevention: Increasing research on strategies to prevent the development of osteopenia in the first place, potentially through early lifestyle interventions.
Conclusion
Osteopenia, once a simple radiological observation, has evolved into a quantifiable state of bone health that affects a significant portion of our aging population. While it represents an increased risk of fractures compared to normal bone density, it's crucial to remember that osteopenia is not a disease in itself, but rather a risk factor that should prompt a comprehensive assessment of fracture risk.
The management of osteopenia in older adults requires a nuanced, personalized approach. By carefully assessing fracture risk, implementing lifestyle modifications, and judiciously using pharmacological interventions when appropriate, we can significantly reduce the burden of fractures in this population.
As research continues to evolve, our approach to osteopenia management will undoubtedly become more refined and effective. For now, the key lies in striking the right balance: addressing the very real risks associated with osteopenia without unnecessarily medicalizing a common condition of aging.
By staying informed about the latest evidence and guidelines, healthcare providers can help their patients navigate the complex landscape of bone health, empowering them to make informed decisions about their care and ultimately reducing the impact of fractures on our aging population.
Remember, when it comes to osteopenia, one size does not fit all. The goal is not just to treat a number on a bone density scan, but to improve overall health, maintain independence, and enhance the quality of life for our older adults.
FAQs
1. What is the difference between osteopenia and osteoporosis?
Both osteopenia and osteoporosis are conditions characterized by low bone density. However, osteopenia is a less severe condition with a BMD T-score between -1.0 and -2.5, while osteoporosis is diagnosed with a T-score of -2.5 or lower. Osteopenia increases the risk of fractures, but it's not as severe as osteoporosis.
2. Can osteopenia progress to osteoporosis?
Yes, osteopenia can progress to osteoporosis over time. This is especially true if risk factors for bone loss, such as aging, smoking, or inadequate calcium and vitamin D intake, are present.
3. How is osteopenia diagnosed?
Osteopenia is typically diagnosed through a bone density scan, usually a DEXA scan. This test measures bone mineral density and compares it to the bone density of a healthy young adult.
4. What are the symptoms of osteopenia?
Osteopenia often has no symptoms in the early stages. However, as bone density decreases and the risk of fractures increases, symptoms may include:
Back pain
Height loss
Fractures (especially in the wrist, hip, or spine)
5. Are there lifestyle changes that can help prevent or manage osteopenia?
Yes, lifestyle changes can significantly improve bone health and reduce the risk of fractures. These include:
Regular weight-bearing exercise: Activities like walking, jogging, dancing, or weightlifting can help strengthen bones.
Balanced diet: Ensure you're getting enough calcium and vitamin D.
Avoid smoking and excessive alcohol consumption: These can harm bone health.
Fall prevention: Take steps to reduce the risk of falls, such as removing tripping hazards and installing grab bars.
6. Are there medications to treat osteopenia?
For individuals with a high risk of fractures, medications like bisphosphonates may be prescribed. These medications can help slow bone loss and reduce the risk of fractures.
7. How often should I get a bone density scan?
The frequency of bone density scans depends on your individual risk factors and treatment plan. Your doctor will determine the best schedule for you.
8. Is osteopenia a concern for men as well as women?
Yes, osteopenia can affect both men and women. However, it is more common in women, especially after menopause.
9. Can I reverse osteopenia?
While it's generally not possible to completely reverse osteopenia, lifestyle changes and medications can help slow bone loss and reduce the risk of fractures.
10. What are the long-term consequences of untreated osteopenia?
Untreated osteopenia can lead to an increased risk of fractures, which can result in pain, disability, and even death.
Related Article
Osteoporosis and Sarcopenia: The Impact of Osteoporosis on Muscle Health
Journal reference
Reid, I. R., & McClung, M. R. (2024). Osteopenia: A key target for fracture prevention. The Lancet Diabetes & Endocrinology. https://doi.org/10.1016/S2213-8587(24)00225-0
Image credit: https://www.frontiersin.org/files/Articles/687037/fimmu-12-687037-HTML/image_m/fimmu-12-687037-g001.jpg
Disclaimer
The information on this website is for informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health care provider with any questions you may have regarding a medical condition or treatment. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
