Removal of Both Ovaries (Bilateral Oophorectomy) Before Menopause linked to Long Term Health Risks
Considering removing your ovaries? Understand the potential long-term health risks, including increased chronic conditions and reduced physical function, especially if done before age 46. This study offers insights for informed decision-making.
DR T S DIDWAL MD
2/26/20246 min read
According to a study in the journal Menopause Women who had their ovaries removed before age 46 (PBO) were more likely to develop chronic conditions like arthritis, asthma, and sleep apnea later in life compared to women who hadn't undergone the surgery. They also walked shorter distances, indicating a potential physical decline. While PBO between 46-49 also increased some risks, the effects were less severe. Cognitive function didn't seem significantly affected in any group. This study suggests PBO, especially before age 46, might have negative long-term health consequences.
Key Findings
PBO, the removal of both ovaries, is often performed alongside a hysterectomy (removal of the uterus).
Traditionally, PBO was done to prevent ovarian cancer in women at average risk, but concerns have arisen about its long-term effects.
Ovaries produce important hormones and their removal can disrupt various body functions.
Study Design:
Researchers compared 274 women who had PBO with or without hysterectomy to 240 women who hadn't undergone the surgery (referent group).
Participants were all aged 55 or older and the average follow-up time was 22 years after PBO.
Women in the PBO group were divided into two categories: those who had the surgery before age 46 and those who had it between ages 46-49.
Results:
Women who had PBO before age 46 had a higher risk of developing the following conditions compared to the referent group:
Arthritis
Asthma
Obstructive sleep apnea
Bone fractures
They also walked a shorter distance during a physical function test.
Women who had PBO between ages 46-49 only had a higher risk of developing arthritis and obstructive sleep apnea compared to the referent group.
There were no significant differences in cognitive function between any of the groups.
Conclusion:
This study suggests that PBO, especially when performed before age 46, can have negative long-term health consequences for women. These include an increased risk of developing various chronic conditions and potentially reduced physical function. However, cognitive function seems .
In this comprehensive analysis, we delve into the intricate relationship between prophylactic bilateral oophorectomy (PBO), with or without concurrent or preceding hysterectomy, and its implications on chronic conditions, cognitive status, and physical function among women, particularly those at a median age of 67 years. Our exploration sheds light on crucial findings that highlight the potential long-term effects of PBO, emphasizing the need for informed decision-making, especially among women with benign gynecologic conditions or those considering ovarian cancer prevention.
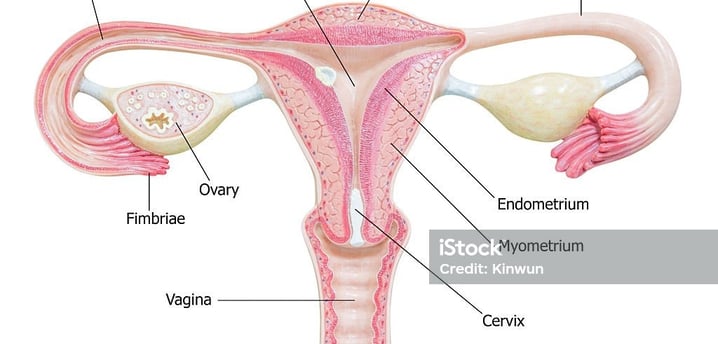
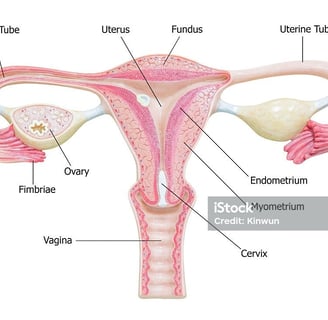
Understanding the Procedures: Bilateral Oophorectomy and Hysterectomy
Before delving into the long-term effects, it's essential to understand the procedures at the heart of this matter. A bilateral oophorectomy involves the surgical removal of both ovaries, while a hysterectomy entails the removal of the uterus. These surgeries can be performed separately or combined, depending on the patient's condition and medical requirements.
Immediate Changes: Hormonal Impact
Following a premenopausal bilateral oophorectomy, a woman's body undergoes a dramatic hormonal shift. The ovaries are the primary source of estrogen and progesterone production, and their removal can induce an abrupt onset of menopause. This immediate hormonal alteration can lead to hot flashes, mood swings, and other menopausal symptoms.
Physical Aging: Skin, Bones, and Heart Health
Skin Health
Estrogen, the hormone predominantly produced by the ovaries, plays a pivotal role in maintaining skin elasticity and hydration. Its decline due to oophorectomy can accelerate the appearance of wrinkles and skin dryness. Additionally, reduced collagen production may contribute to a loss of skin firmness over time.
Bone Health
Estrogen also influences bone density and strength. Post-oophorectomy, women may face an increased risk of osteoporosis, a condition characterized by fragile bones prone to fractures. This underscores the importance of proactive measures like calcium and vitamin D supplementation, along with weight-bearing exercises, to mitigate this risk.
Heart Health
Estrogen's protective effect extends to the cardiovascular system. It helps maintain healthy cholesterol levels and blood vessel function. Consequently, women who undergo oophorectomy may have a heightened risk of heart disease in the long run. Lifestyle modifications, such as a heart-healthy diet and regular exercise, become imperative.
Chronic Medical Conditions: Cancer Risk and Cognitive Health
Cancer Risk
One of the primary reasons for these surgeries is the prevention or treatment of certain cancers, such as ovarian and uterine cancer. However, the removal of ovaries may increase the risk of other cancers, like breast cancer. The decision to undergo these procedures should be made in consultation with a healthcare provider, considering individual cancer risk factors.
Cognitive Health
Emerging research is shedding light on the potential link between hormonal changes induced by oophorectomy and cognitive health. Some studies suggest that a lack of estrogen may be associated with a higher risk of cognitive decline and conditions like Alzheimer's disease. Further research is needed to fully understand this complex relationship.
Quality of Life: Emotional and Sexual Well-being
Emotional Well-being
The abrupt hormonal changes following oophorectomy can lead to mood swings, anxiety, and depression. Healthcare providers must address these emotional aspects and provide appropriate support, including counseling and medication, when necessary.
Sexual Well-being
Estrogen also plays a crucial role in maintaining vaginal health and sexual function. Its decline can lead to vaginal dryness and discomfort during intercourse. Open communication with healthcare providers can help women manage these issues and explore available treatment options.
Increased Odds of Chronic Conditions
Women subjected to PBO, whether accompanied by hysterectomy or not, exhibited heightened odds of various chronic conditions compared to their counterparts who did not undergo such procedures. Specifically, arthritis, chronic obstructive pulmonary disease (COPD), and obstructive sleep apnea surfaced as notable conditions with increased prevalence among women who underwent PBO. Furthermore, age at PBO emerged as a significant factor, with early PBO correlating with augmented odds of arthritis, asthma, bone fractures, and obstructive sleep apnea. These findings underscore the importance of considering the timing of PBO, especially in relation to the onset of chronic conditions.
Consistency with Previous Studies
Our investigation aligns with prior research, notably the extensive MOA-2 study, in elucidating associations between PBO and the development of cardiovascular diseases, strokes, arthritis, asthma, COPD, and the accumulation of multiple chronic conditions. The parallelism in results between our study subset and the broader MOA-2 study reaffirms the robustness of the observed associations, particularly emphasizing the elevated risks associated with early PBO.
Cognitive Status and Physical Function
Contrary to some previous findings, our study did not establish a direct association between PBO and diagnosed mild cognitive impairment (MCI) or dementia. However, our findings do not negate the potential impact of PBO on cognitive function, especially considering the prevalence of subjective cognitive decline among younger women subjected to PBO. Moreover, our exploration into physical function revealed a consistent pattern, with early PBO correlating with diminished performance in the 6-minute walk test, suggesting subtle yet significant alterations in physical capabilities following the procedure.
Body Composition Changes
An intriguing aspect of our study pertains to the changes in body composition following PBO, particularly alterations in BMI, fat mass, and lean mass. Notably, earlier PBO was correlated with greater changes in fat mass, indicating potential metabolic shifts post-procedure. Understanding these changes is crucial for comprehensive post-operative care and long-term health management among women undergoing PBO.
Unraveling the Mechanisms
While the precise mechanisms linking PBO to somatic aging and chronic conditions remain elusive, hypotheses revolving around hormonal alterations, inflammation, cellular senescence, and mitochondrial dysfunction warrant further exploration. Future studies dissecting these mechanisms hold promise in elucidating the intricacies of PBO's impact on women's health.
Strengths and Limitations
Our study benefits from comprehensive in-person assessments and a representative sample from a well-defined population. However, inherent limitations, including the cross-sectional design, participation bias, and limited generalizability, underscore the need for cautious interpretation of results and warrant further longitudinal investigations.
To Summarize
Increased chronic conditions: Women who underwent PBO, especially before age 46, were more likely to develop chronic conditions like arthritis, asthma, and sleep apnea later in life compared to those who didn't have the surgery.
Age matters: Early PBO (before age 46) had a stronger association with increased risks of chronic conditions compared to PBO done at a later age.
Cognitive function: This study did not find a direct link between PBO and diagnosed cognitive decline. However, it highlights the need for further research on the potential impact of PBO on cognitive function, especially in younger women.
Physical function: Early PBO was associated with reduced performance in a physical function test, suggesting a potential decline in physical abilities after the procedure.
Body composition: Women who had PBO earlier experienced greater changes in body fat distribution, indicating potential metabolic shifts.
Conclusion: Informed Decision-making
In the realm of women's health, the decision to undergo premenopausal bilateral oophorectomy with or without hysterectomy is a complex and deeply personal one. It involves weighing the immediate benefits, such as cancer risk reduction, against the long-term effects on physical aging, chronic medical conditions, and overall quality of life. Women considering these procedures must engage in open and thorough discussions with their healthcare providers. Individualized assessments of cancer risk, consideration of alternative treatments, and strategies to mitigate the long-term effects should all be part of the decision-making process.
Reference:
Mielke, M. M., Kapoor, E., Geske, J. R., Fields, J. A., LeBrasseur, N. K., Morrow, M. M., Winham, S. J., Faubion, L. L., Castillo, A. M., Hofrenning, E. I., Bailey, K. R., Rocca, W. A., & Kantarci, K. (2023, September 11). Long-term effects of premenopausal bilateral oophorectomy with or without hysterectomy on physical aging and chronic medical conditions. Menopause, 30(11), 1090–1097. https://doi.org/10.1097/gme.000000000000225
Related:
Medical Disclaimer
The information on this website is for informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health care provider with any questions you may have regarding a medical condition or treatment. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
