Stronger Bones Through Resistance Training: The One Exercise You’re Missing
Wondering how to truly fortify your bones? This comprehensive resistance training guide reveals a key exercise and provides practical applications, from intensity and frequency to optimal exercises for all ages. Start building stronger bones today!
DR T S DIDWAL MD
5/6/20259 min read

The Ultimate Guide to Resistance Training for Bone Health: Scientific Evidence and Practical Applications
In an era where living longer has become the norm, the question of how we maintain our skeletal integrity as we age has never been more critical. Among the various interventions available, resistance training stands out as a powerful tool for enhancing bone health and promoting longevity. This comprehensive guide delves into the science behind how lifting weights and other forms of resistance exercise can strengthen your bones, prevent fractures, and contribute to overall healthspan.
Understanding Bone as a Dynamic Tissue
Before we explore the benefits of resistance training, it's essential to understand that bone tissue isn't static. Contrary to what many believe, your bones aren't inert structures but rather highly dynamic tissues that continuously undergo a process called remodeling.
This remodeling is orchestrated by two main types of cells:
Osteoblasts: Responsible for building new bone
Osteoclasts: Responsible for breaking down old bone
The balance between these cellular activities determines whether you gain, maintain, or lose bone mass over time. As we age, this balance typically shifts toward greater resorption (breakdown) than formation, leading to a net loss of bone mineral density (BMD).
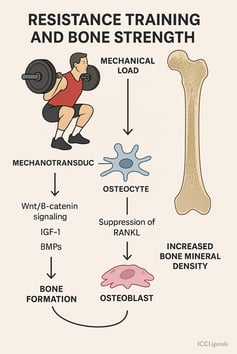
The Biological Mechanism: How Mechanical Loading Strengthens Bones
When you perform resistance exercises, you create mechanical forces that act upon your skeletal system. This mechanical loading triggers a fascinating biological response known as mechanotransduction – the process by which physical forces are converted into biochemical signals within bone cells.
Wolff's Law and Bone Adaptation
The fundamental principle governing bone adaptation to mechanical loads is known as Wolff's Law, which postulates that bone adapts to the loads placed upon it. According to this principle, when bones experience appropriate stress through resistance training, they respond by becoming stronger and denser.
Mechanosensitive cells called osteocytes act as the bone's strain detectors. When these cells sense mechanical strain during resistance exercises, they trigger signaling pathways that activate osteoblasts to form new bone tissue. This process ultimately enhances bone mineral density (BMD) and structural integrity.
Molecular Pathways of Bone Formation
At the molecular level, resistance training activates several key pathways that promote bone formation:
Wnt/β-catenin signaling pathway: A critical regulator of osteoblast differentiation and bone formation
Bone morphogenetic proteins (BMPs): Growth factors that stimulate osteogenesis
Insulin-like growth factor-1 (IGF-1): An anabolic hormone that promotes bone growth
Suppression of RANKL signaling: Reduces osteoclastic bone resorption
These molecular mechanisms collectively shift the balance in favor of bone accrual rather than breakdown.
Scientific Evidence: What Research Tells Us About Resistance Training and Bone Health
Multiple studies have investigated the effects of resistance training on bone health across different populations. Let's examine some of the key research findings.
Comprehensive Analysis of Bone Adaptation to Resistance Training
A comprehensive article reviewed in our research highlights that resistance training exerts mechanical loading forces that stimulate osteogenic activity, enhancing BMD and structural integrity. The research demonstrates that high-intensity resistance exercises, particularly multi-joint movements like squats, deadlifts, and presses, generate axial loading forces that effectively promote osteogenesis.
The evidence is particularly compelling for postmenopausal women, a demographic highly susceptible to osteoporosis. Compared to non-weight-bearing aerobic activities, resistance training provides superior osteogenic stimuli, leading to measurable improvements in bone mass and microarchitecture.
Comparison of Training Modalities in Older Adults with Low Skeletal Muscle Mass
One significant study compared the effects of two strength training modalities—hypertrophy versus contrast training—on bone health parameters in older adults with low skeletal muscle mass index (SMI). The six-month intervention involved 41 participants divided into three groups: a control group, a contrast training group (performing movements at high speed), and a hypertrophy training group (performing movements at spontaneous speed).
While both training modalities showed benefits in improving maximal strength, physical performance, and quality of life parameters, neither had significant effects on bone mineral density (BMD) or bone mineral content (BMC) within the six-month timeframe. Interestingly, the contrast training group demonstrated more marked improvements in maximal strength and reduced fracture risk compared to the hypertrophy training group.
Effects of Heavy vs. Moderate Intensity Resistance Training
Another notable study, the LISA (LIve active Successful Aging) study, examined whether bone health was positively influenced by one year of supervised resistance training at different intensities. The study randomized 451 older adults at retirement age to either heavy resistance training (HRT), moderate intensity training (MIT), or a non-exercising control group (CON).
The researchers assessed bone mineral density at the whole body level, femoral neck, and lumbar spine, along with biomarkers of bone degradation and formation. Interestingly, the study found that heavy resistance training positively influenced short-term bone formation in well-functioning older adults, although this effect wasn't maintained at long-term follow-ups. The minor changes in bone biomarkers weren't reflected in changes in BMD measured with DXA scans.
Precision Health Management and Physical Rehabilitation
A study on elderly patients with osteoporosis explored the impact of precision health management coupled with physical rehabilitation on bone biomarkers. Two hundred and forty individuals diagnosed with senile osteoporosis were randomly assigned to either receive personalized health care along with physical therapy or standard health care.
Following the intervention, the precision health management group exhibited significantly reduced pain levels and parathyroid hormone (PTH) levels at 6, 12, 18, and 24 months compared to the control group. Additionally, scores on osteoporosis knowledge, self-efficacy, bone mineral density, alkaline phosphatase (ALP) levels, and calcium levels were significantly higher in the observation group.
Exercise Interventions for Athletes in Low-Impact Sports
A scoping review identified potential exercise interventions that could improve bone health in athletes participating in low-impact sports such as cycling and swimming, who are at increased risk for low bone mineral density. The review found that resistance training, plyometric exercises, whole-body vibration, and combined jumping exercise with collagen supplementation showed promising results in improving bone mineral density in these athletes.
Practical Applications: Designing an Effective Resistance Training Program for Bone Health
Based on the scientific evidence, here are practical guidelines for implementing a bone-strengthening resistance training program:
Key Training Parameters
Intensity: Moderate to high (70-85% of one-repetition maximum)
Frequency: 2-3 sessions per week
Volume: 2-3 sets of 8-12 repetitions per exercise
Exercise Selection: Prioritize multi-joint, weight-bearing exercises
Progression: Gradually increase resistance to maintain the osteogenic stimulus
Optimal Exercises for Bone Health
Upper Body Exercises:
Overhead press
Bench press
Rows
Push-ups
Lower Body Exercises:
Squats
Lunges
Deadlifts
Step-ups
Core and Full-Body Exercises:
Plank variations
Farmer's carries
Kettlebell swings
Implementation Strategies for Different Populations
For Older Adults (65+):
Begin with bodyweight exercises
Progress to resistance bands and light weights
Focus on functional movements that enhance daily activities
Incorporate balance training
For Middle-Aged Adults (40-65):
Moderate to heavy resistance training
Emphasis on proper technique and form
Mix of traditional strength training and power exercises
Consider periodization to avoid plateaus
For Young Adults (20-40):
Higher intensity resistance training
More advanced exercise variations
Greater emphasis on progressive overload
Can incorporate plyometric elements
Special Considerations for Specific Populations
Postmenopausal Women
Postmenopausal women experience accelerated bone loss due to declining estrogen levels. For this demographic:
Start with lower intensities and gradually progress
Include exercises specifically targeting the spine and hip—common fracture sites
Consider combining resistance training with weight-bearing aerobic activities
Emphasize proper technique to avoid injury
Older Adults with Sarcopenia
For older adults with age-related muscle loss (sarcopenia):
Focus on resistance training that addresses both muscle and bone health
Implement contrast training (as suggested by research) for potentially greater benefits
Include exercises that enhance functional strength and balance
Consider supervised training to ensure proper form and safety
Athletes in Low-Impact Sports
For swimmers, cyclists, and other athletes in non-weight-bearing sports:
Incorporate resistance training 2-3 times per week
Add plyometric exercises for greater osteogenic stimulus
Consider whole-body vibration training as a supplement
Implement jumping exercises with proper progression
Nutritional Support for Maximizing Bone Adaptations
Resistance training's bone-building effects can be optimized with proper nutrition:
Essential Nutrients for Bone Health
Calcium: The primary mineral in bone (1000-1200 mg/day for adults)
Vitamin D: Critical for calcium absorption (600-800 IU/day)
Protein: Provides amino acids for bone matrix formation (1.2-1.6 g/kg body weight)
Magnesium: Important for bone mineralization (310-420 mg/day)
Vitamin K: Necessary for bone protein synthesis (90-120 mcg/day)
Timing of Nutrient Intake
Consume protein within 1-2 hours after resistance training
Distribute calcium intake throughout the day for optimal absorption
Consider vitamin D supplementation if sun exposure is limited
Monitoring Progress and Evaluating Bone Health
To track the effectiveness of your resistance training program on bone health:
Assessment Methods
Dual-Energy X-ray Absorptiometry (DXA): Gold standard for measuring BMD
Biochemical Markers: Blood tests for markers of bone formation (P1NP) and resorption (CTX)
Functional Assessments: Tests of balance, strength, and functional capacity
Reasonable Expectations
It's important to set realistic expectations:
Significant changes in BMD typically require 6-12 months of consistent training
Initial adaptations may occur at the biochemical level before detectable changes in BMD
The primary goal may be preventing bone loss rather than substantial gains in bone mass
Common Challenges and Solutions
Overcoming Barriers to Resistance Training
Challenge: Fear of injury Solution: Start with supervised sessions to learn proper technique
Challenge: Lack of access to equipment Solution: Utilize bodyweight exercises or resistance bands
Challenge: Uncertainty about program design Solution: Consult with a qualified exercise professional for a personalized plan
Maintaining Long-Term Adherence
To sustain a bone-strengthening resistance training program:
Find activities you enjoy
Train with partners or in group settings
Track progress to maintain motivation
Periodically change your routine to prevent boredom
FAQs About Resistance Training and Bone Health
Is resistance training safe for individuals with osteoporosis?
Yes, but with appropriate modifications. Individuals with diagnosed osteoporosis should work with healthcare providers and qualified exercise professionals to design a safe program. Generally, exercises should avoid excessive spine flexion and focus on stability and controlled movements.
How long does it take to see improvements in bone health from resistance training?
Biochemical changes may occur within weeks, but measurable changes in bone mineral density typically require at least 6-12 months of consistent training. For some individuals, especially those with established osteoporosis, the primary benefit may be slowing bone loss rather than significantly increasing bone mass.
Can resistance training reverse osteoporosis?
While resistance training alone may not completely reverse established osteoporosis, it can slow bone loss and, in some cases, lead to modest improvements in bone mineral density. Combined with proper nutrition and medication (if prescribed), resistance training is a vital component of osteoporosis management.
Is high-intensity training better than moderate-intensity training for bone health?
Research suggests that higher intensities generally provide greater osteogenic stimulus. However, the optimal approach depends on individual factors such as age, current bone health, fitness level, and exercise experience. For many people, a progressive approach starting with moderate intensity and gradually increasing is safest and most effective.
How does resistance training compare to other forms of exercise for bone health?
Resistance training and high-impact activities (like jumping) provide the strongest stimuli for bone formation. Weight-bearing aerobic activities (walking, jogging) offer moderate benefits, while non-weight-bearing activities (swimming, cycling) provide minimal direct benefit to bone health.
Can I improve bone health with resistance bands or bodyweight exercises?
Yes, although the osteogenic stimulus may be less than with free weights or machines. The key is to ensure that the exercises provide progressive overload. As you adapt, you'll need to increase resistance by using stronger bands or more challenging bodyweight exercise variations.
Key Takeaways
Bone is living tissue that adapts to mechanical loading through the process of mechanotransduction.
Resistance training stimulates osteoblast activity and suppresses osteoclast function, shifting the balance toward bone formation.
Multi-joint, weight-bearing exercises that load the axial skeleton provide the most effective osteogenic stimulus.
Training parameters matter: moderate to high intensity, progressive overload, and consistent frequency are crucial for bone adaptations.
Different populations (older adults, postmenopausal women, athletes) may require specific approaches to maximize bone health benefits.
Nutritional support, particularly adequate calcium, vitamin D, and protein, enhances the bone-building effects of resistance training.
Monitoring progress through appropriate assessments helps track bone health improvements and guide program adjustments.
Patience is essential: significant bone adaptations may take 6-12 months or longer to manifest.
Call to Action
Don't wait until bone loss becomes a problem—start strengthening your skeletal system today through resistance training:
Consult with healthcare providers before beginning a new exercise program, especially if you have existing bone health concerns.
Work with qualified exercise professionals to design a bone-strengthening resistance training program tailored to your needs and goals.
Start where you are with appropriate exercises and gradually progress as your strength and confidence improve.
Be consistent with your training—bone adaptations require regular stimulus over time.
Combine resistance training with proper nutrition to provide your body with the building blocks for strong bones.
Consider comprehensive bone health testing to establish a baseline and track your progress.
Remember, investing in your bone health today through resistance training will pay dividends in mobility, independence, and quality of life for decades to come. Your skeleton is the framework upon which all movement depends—give it the strength it deserves!
Related Article
Are You Training Right? The Science of Resistance Training Explained | Healthnewstrend
Citations
Cui, Y., Xu, Z., Cui, Z., Guo, Y., Wu, P., & Zhou, X. (2025). Association between life’s essential 8 and bone mineral density among adults aged 20–59 years. Scientific Reports, 15(1), 1-10. https://doi.org/10.1038/s41598-025-86749-7
Bloch-Ibenfeldt, M., Gates, A. T., Jørgensen, N. R., Linneberg, A., Aadahl, M., Kjær, M., & Boraxbekk, C. J. (2025). Heavy resistance training provides short-term benefits on bone formation in well-functioning older adults. Bone, 193, 117393. https://doi.org/10.1016/j.bone.2025.117393
Antoun, A., Watelain, E., Pinti, A., Khalil, N., Berro, A., Maliha, E., Bassim, Y., & El Hage, R. (2025). Influence of two strength training modalities (hypertrophy vs. Contrast training) on muscular strength, bone health parameters and quality of life in a group of older adults with low skeletal muscle mass index. Journal of Clinical Densitometry, 28(2), 101563. https://doi.org/10.1016/j.jocd.2025.101563
Chen, L., Yan, X., Liu, Y., Pei, Y., Zhou, J., Zhang, L., & Du, Z. (2025). Effect of precise health management combined with physical rehabilitation on bone biomarkers in senile osteoporosis patients. Scientific Reports, 15(1), 1-9. https://doi.org/10.1038/s41598-025-86188-4
Florvåg, A.G., Berg, Ø.A., Røksund, O.D. et al. Exercise interventions to improve bone mineral density in athletes participating in low-impact sports: a scoping review. BMC Musculoskelet Disord 26, 73 (2025). https://doi.org/10.1186/s12891-025-08316-5
Haque, I., Schlacht, T. Z., & Skelton, D. A. (2024). The effects of high velocity resistance training on bone mineral density in older adults: A systematic review. Bone, 179, 116986. https://doi.org/10.1016/j.bone.2023.116986
Disclaimer
The information on this website is for informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health care provider with any questions you may have regarding a medical condition or treatment. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
About the Author:
Dr.T.S. Didwal, MD, is an experienced Internal Medicine Physician with over 30 years of practice. Specializing in internal medicine, he is dedicated to promoting wellness, preventive health, and fitness as core components of patient care. Dr. Didwal’s approach emphasizes the importance of proactive health management, encouraging patients to adopt healthy lifestyles, focus on fitness, and prioritize preventive measures. His expertise includes early detection and treatment of diseases, with a particular focus on preventing chronic conditions before they develop. Through personalized care, he helps patients understand the importance of regular health screenings, proper nutrition, exercise, and stress management in maintaining overall well-being.
