Testosterone to Estradiol Ratio: Hormonal Imbalance Linked to Metabolic Syndrome in Men
A recent study reveals that the testosterone to estradiol ratio in men is a strong predictor of metabolic syndrome. This health condition increases the risk of heart disease, stroke, and type 2 diabetes. Learn how hormonal imbalances can affect your overall health and what you can do to manage metabolic syndrome.
DR T S DIDWAL MD
9/24/20248 min read
The research published in the Archives of Razi Institute highlights the intricate relationship between sex hormones and metabolic syndrome (MetS) in men. It found that men with MetS have lower testosterone levels and higher estradiol levels, leading to a lower testosterone-to-estradiol ratio. This ratio can be a predictor of MetS, indicating the condition's likelihood. The study also explored the vicious cycle between obesity and hormonal imbalance, where increased fat tissue promotes estradiol production, further contributing to MetS. The findings have implications for diagnosis and treatment, suggesting the need for incorporating hormonal assessments into screening protocols and tailoring treatment plans based on individual hormonal profiles. Lifestyle interventions, including weight management, exercise, healthy diet, stress management, and adequate sleep, remain crucial for preventing and managing MetS. Future research may focus on hormone-based therapies, personalized medicine, novel biomarkers, and lifestyle interventions to address this complex health issue.
Key points
Metabolic Syndrome (MetS) is a cluster of metabolic abnormalities that increase the risk of cardiovascular disease and type 2 diabetes.
Men with MetS have lower testosterone levels and higher estradiol levels, leading to a lower testosterone to estradiol ratio.
The testosterone to estradiol ratio can be a predictor of MetS, indicating the likelihood of the condition.
Obesity and hormonal imbalance create a vicious cycle, where increased fat tissue promotes estradiol production, further contributing to MetS.
The findings have implications for diagnosis and treatment, suggesting the need for incorporating hormonal assessments into screening protocols and tailoring treatment plans based on individual hormonal profiles.
Lifestyle interventions remain crucial for preventing and managing MetS, including weight management, exercise, healthy diet, stress management, and adequate sleep.
Future research may focus on hormone-based therapies, personalized medicine, novel biomarkers, and lifestyle interventions to address MetS.
Understanding Metabolic Syndrome and the Role of Sex Hormones in Men
Metabolic syndrome (MetS) has become a global health challenge affecting both developed and developing countries. This complex condition, characterized by a cluster of metabolic abnormalities, significantly increases the risk of cardiovascular disease and type 2 diabetes. Recent research has shed light on the intricate relationship between sex hormones and MetS in men, offering new insights into potential diagnostic and preventive strategies.
What is Metabolic Syndrome?
Metabolic syndrome, also known as syndrome X or insulin resistance syndrome, is a collection of metabolic disorders that occur together, increasing your risk of heart disease, stroke, and type 2 diabetes. The condition is diagnosed when a person has at least three of the following five metabolic risk factors:
Central obesity (excess fat around the waist)
High blood pressure
High blood sugar
High triglyceride levels
Low levels of high-density lipoprotein (HDL) cholesterol (the "good" cholesterol)
The prevalence of MetS varies globally, affecting about one-fifth of the American population and a quarter of the European population. In the Middle East, including Iraq, the prevalence is particularly high, reaching up to 46.6% in some studies.
The Link Between Sex Hormones and Metabolic Syndrome in Men
Recent research has uncovered a fascinating connection between sex hormones and metabolic syndrome in men. A study conducted in Iraq aimed to evaluate the ratio of total testosterone (TT) to estradiol (E2) as a potential predictor of MetS. The findings were enlightening and could have significant implications for how we approach the diagnosis and management of MetS in men.
Key Findings of the Study
Lower Testosterone Levels: Men with metabolic syndrome had significantly lower levels of total testosterone compared to healthy individuals.
Higher Estradiol Levels: Conversely, estradiol levels were significantly higher in men with MetS.
Testosterone to Estradiol Ratio: The ratio of testosterone to estradiol was markedly lower in men with MetS, suggesting this ratio could be a valuable predictor of the condition.
Correlation with MetS Components: The TT to E2 ratio showed significant correlations with various components of metabolic syndrome, including waist circumference, blood pressure, fasting blood glucose, and lipid profile.
Understanding the Hormonal Imbalance
The hormonal imbalance observed in men with metabolic syndrome is not just a coincidence but likely plays a crucial role in the development and progression of the condition. Here's how these hormonal changes might contribute to MetS:
The Role of Testosterone
Testosterone, the primary male sex hormone, plays several important roles in metabolic health:
It helps maintain muscle mass, which is crucial for metabolic rate and insulin sensitivity.
It promotes the distribution of fat away from the abdominal area.
It supports cardiovascular health and helps regulate blood sugar levels.
When testosterone levels are low, as observed in men with MetS, these protective effects are diminished, potentially contributing to the development of metabolic abnormalities.
The Impact of Elevated Estradiol
While estradiol (a form of estrogen) is present in men in small amounts, elevated levels can have negative metabolic effects:
It can promote fat accumulation, particularly in the abdominal area.
High levels may contribute to insulin resistance.
It might influence lipid metabolism, potentially leading to unfavorable changes in cholesterol levels.
The combination of low testosterone and high estradiol creates a hormonal environment that appears to be conducive to the development of metabolic syndrome.
The Testosterone to Estradiol Ratio as a Predictor
One of the most intriguing findings of the study was the potential use of the testosterone-to-estradiol ratio as a predictor of metabolic syndrome. The researchers identified a cutoff point for this ratio that showed promising results in predicting MetS:
A TT to E2 ratio of 8.4 or lower was found to be predictive of MetS.
The overall accuracy of this predictor was 78.9%.
These findings suggest that the TT to E2 ratio could be a valuable tool for healthcare providers in assessing a man's risk of metabolic syndrome.
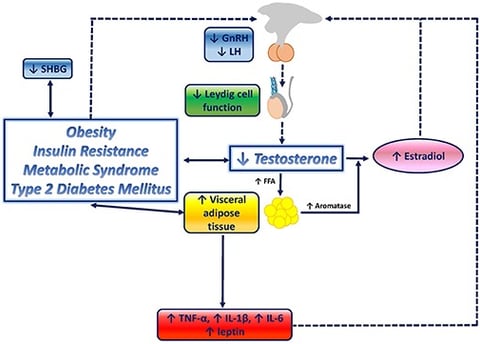
The Vicious Cycle of Obesity and Hormonal Imbalance
The study's findings also highlight a potentially vicious cycle between obesity (a key component of MetS) and hormonal imbalance:
Increased Fat Tissue: As men gain weight, particularly around the abdomen, fat tissue increases.
Aromatase Activity: Fat tissue contains an enzyme called aromatase, which converts testosterone to estradiol.
Hormonal Shift: This leads to a decrease in testosterone and an increase in estradiol.
Metabolic Effects: The resulting hormonal imbalance may further promote fat accumulation and insulin resistance, exacerbating the metabolic syndrome.
Cycle Continues: As the metabolic syndrome worsens, it can further impact hormonal balance, creating a self-perpetuating cycle.
Understanding this cycle is crucial for developing effective interventions to break it and improve metabolic health.
Implications for Diagnosis and Treatment
The findings of this study have several important implications for the diagnosis and treatment of metabolic syndrome in men:
Enhanced Screening
Incorporating hormonal assessments, particularly the TT to E2 ratio, into screening protocols for MetS could help identify at-risk individuals earlier. This could lead to more timely interventions and potentially prevent the progression of the condition.
Personalized Treatment Approaches
Understanding a patient's hormonal profile could help healthcare providers tailor treatment approaches. For example, men with low testosterone might benefit from hormone replacement therapy as part of their MetS management plan.
Monitoring Treatment Efficacy
The TT to E2 ratio could potentially be used to monitor the efficacy of treatments for MetS. Improvements in this ratio might indicate that interventions are successfully addressing the underlying metabolic disturbances.
Risk Stratification
The hormonal profile could help in risk stratification, allowing healthcare providers to identify which patients with MetS are at the highest risk of complications and require more aggressive management.
Lifestyle Interventions for Metabolic Syndrome
While hormonal imbalances play a significant role in MetS, lifestyle interventions remain the cornerstone of prevention and treatment. Here are some key strategies that can help address both the metabolic and hormonal aspects of the condition:
Weight Management
Losing excess weight, particularly abdominal fat, can have a profound impact on metabolic health and hormonal balance. Even modest weight loss can improve insulin sensitivity, blood pressure, and lipid profiles.
Regular Physical Activity
Exercise is crucial for metabolic health. It can help:
Improve insulin sensitivity
Reduce abdominal fat
Increase muscle mass
Boost testosterone levels
Improve cardiovascular health
Aim for at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity aerobic activity per week, along with strength training exercises.
Balanced Diet
A healthy diet is essential for managing MetS. Focus on:
Whole grains
Lean proteins
Healthy fats (e.g., olive oil, avocados, nuts)
Plenty of fruits and vegetables
Limiting processed foods, sugary drinks, and excessive alcohol
Stress Management
Chronic stress can contribute to hormonal imbalances and metabolic disturbances. Incorporate stress-reduction techniques such as meditation, yoga, or deep breathing exercises into your daily routine.
Adequate Sleep
Poor sleep can negatively impact hormonal balance and metabolic health. Aim for 7-9 hours of quality sleep each night.
The Future of Metabolic Syndrome Management
The discovery of the relationship between sex hormones and metabolic syndrome opens up new avenues for research and treatment. Future studies may focus on:
Hormone-Based Therapies: Investigating whether hormone replacement or modulation therapies can effectively treat or prevent MetS in men.
Personalized Medicine: Developing personalized treatment plans based on an individual's hormonal profile and genetic factors.
Novel Biomarkers: Identifying additional biomarkers that, in combination with hormonal assessments, could improve the prediction and diagnosis of MetS.
Lifestyle Interventions: Researching how specific lifestyle interventions affect both hormonal balance and metabolic health.
Conclusion
Metabolic syndrome represents a significant health challenge, but our understanding of its underlying mechanisms continues to grow. The discovery of the relationship between sex hormones and MetS in men provides new insights that could revolutionize how we approach this condition.
By considering hormonal factors, particularly the testosterone to estradiol ratio, healthcare providers may be able to identify at-risk individuals earlier and implement more effective, personalized treatment strategies. However, it's important to remember that while hormonal assessments can be valuable, they should be used in conjunction with traditional diagnostic criteria and as part of a comprehensive approach to metabolic health.
For individuals concerned about their metabolic health, the message remains clear: maintaining a healthy weight, staying physically active, eating a balanced diet, managing stress, and getting adequate sleep are powerful tools for preventing and managing metabolic syndrome. As research in this field progresses, we can look forward to even more targeted and effective strategies for combating this pervasive health issue.
Remember, if you're concerned about your risk of metabolic syndrome, consult with your healthcare provider. They can assess your individual risk factors, including hormonal balance, and work with you to develop a personalized plan for optimal metabolic health.
Faqs
Does low sex hormone-binding globulin cause metabolic syndrome in nonobese men?
While low sex hormone-binding globulin (SHBG) is associated with metabolic syndrome (MetS) in nonobese men, it's not the sole cause. The relationship is complex and likely involves a combination of factors, including reduced testosterone levels, insulin resistance, and other metabolic disturbances.
Does sex hormone-binding globulin protect against metabolic syndrome?
Yes, higher levels of SHBG are generally associated with a lower risk of MetS. SHBG binds to testosterone, reducing its bioavailability. This can be beneficial in individuals with MetS, as high levels of free testosterone can contribute to the condition. However, it's important to note that the relationship between SHBG and MetS is not always straightforward, and other factors may also play a role.
What causes metabolic syndrome in nonobese men?
Metabolic syndrome in nonobese men can be caused by a variety of factors, including:
Insulin resistance: This is a key factor in MetS, and it can occur even in individuals with a normalbody weight.
Genetics: A family history of MetS or related conditions can increase your risk.
Lifestyle factors: Poor diet, lack of physical activity, excessive alcohol consumption, and chronic stress can contribute to MetS.
Hormonal imbalances: As discussed in the study, low testosterone levels and high estradiol levels can play a role.
Medications: Certain medications, such as corticosteroids and antipsychotics, can increase the risk of MetS.
How can I improve my testosterone levels? Engaging in regular physical activity, maintaining a healthy weight, reducing stress, and getting enough sleep can help boost testosterone levels naturally. In some cases, hormone replacement therapy may be considered.
What are the symptoms of metabolic syndrome? Symptoms may include fatigue, excessive thirst, frequent urination, blurred vision, slow-healing wounds, and difficulty concentrating.
How is metabolic syndrome diagnosed? A healthcare provider will conduct a physical exam and order blood tests to check for elevated blood sugar, high triglycerides, low HDL cholesterol, and high blood pressure.
What is the treatment for metabolic syndrome? Treatment typically involves lifestyle changes, such as healthy eating, regular exercise, and weight management. In some cases, medications may be prescribed to manage blood pressure, blood sugar, or cholesterol levels.
Related Articles
1.Obesity, Waist Circumference and Hormonal Health in Men
2.Is There a Link Between Testosterone Deficiency and Anemia?
Journal Reference
Ali Hamza, M., Abdulhameed, A., & Ali Mansour, A. (2022). Total Testosterone to Estradiol Ratio as a Predictor Marker of Metabolic Syndrome in Males. Archives of Razi Institute, 77(1), 351–357. https://doi.org/10.22092/ARI.2021.356607.1878
Image credit: https://www.frontiersin.org/files/Articles/446821/fendo-10-00345-HTML/image_m/fendo-10-00345-g001.jpg
Disclaimer
The information on this website is for educational and informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition or treatment, and before undertaking a new healthcare regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
