The Autonomic Nervous System & Exercise: Secrets Every Athlete Must Know to Boost Performance & Recovery
Discover how the autonomic nervous system impacts exercise performance, recovery, and sleep. Learn HRV insights, neural signaling secrets, and science-backed strategies every athlete and coach must know.
3/25/20256 min read
Effects of Exercise Training on the Autonomic Nervous System
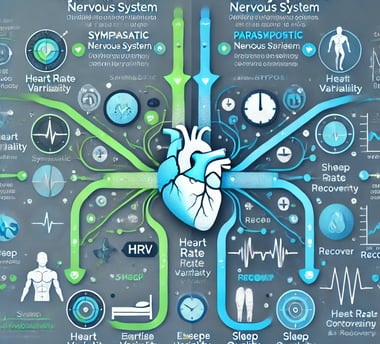
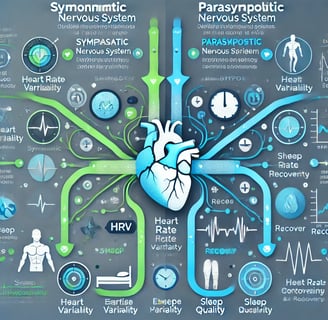
The autonomic nervous system (ANS), comprising the sympathetic (SNS) and parasympathetic (PNS) branches, is vital for maintaining homeostasis. Modern lifestyles, rife with chronic stress, often disrupt this balance, favoring SNS dominance and PNS suppression, leading to ANS dysfunction. This imbalance significantly impacts health, particularly the immune system, cardiovascular, oxidative stress, and metabolic dysregulation.
The hypothalamic-pituitary-adrenal (HPA) axis, alongside the SNS and PNS, modulates immune responses. While the HPA axis and PNS generally exert anti-inflammatory effects, the SNS demonstrates a dual role, exhibiting both pro- and anti-inflammatory actions. Physical exercise (PE), though generally beneficial, can act as a physiological stressor, influencing ANS activity.
Autonomic Nervous System Insights: Revolutionizing Exercise Performance and Health
The autonomic nervous system orchestrates the intricate cardiovascular dance during acute exercise, ensuring oxygen delivery matches metabolic demands. V˙O₂max, a measure of maximal oxygen uptake, hinges on heart rate, stroke volume, and arterial-venous oxygen difference. Both central command and the exercise pressor reflex are pivotal, resetting the arterial baroreflex for precise control. Individuals with autonomic disorders exhibit diminished V˙O₂max and abnormal cardiovascular responses, limiting their physical capacity.
Chronic exercise training emerges as a potent modulator of the autonomic system, offering therapeutic benefits. It enhances vascular function, promotes blood volume expansion, induces favorable cardiac remodeling, and combats insulin resistance. Moreover, exercise positively influences renal-adrenal function and fosters mental well-being, mitigating depression and bolstering self-esteem.
Recommended guidelines advocate for at least 30 minutes of moderate-intensity exercise, five days a week. For those with autonomic disorders, supervised exercise is especially crucial to optimize functional capacity and maximize therapeutic outcomes.
Key Research Findings: A Comprehensive Overview
1. Heart Rate Variability in Football Players: Performance Indicators
A pivotal study examining 25 male football players revealed fascinating insights into HRV as a performance metric:
Aerobic Capacity Correlation: HRV Score showed a positive correlation with VO2max
Neuromuscular Coordination: Mean RR intervals correlated strongly with neuromuscular coordination
Sleep Quality Impact: HRV demonstrated significant relationships with sleep quality
Body Awareness: Researchers found a notable correlation with body awareness.
2. Central Nervous System and Exercise Responses
Cutting-edge research has highlighted the complex interplay between insulin signaling and cardiovascular responses during exercise:
Key Neural Control Mechanisms
Exercise Pressor Reflex (EPR): Mediates circulatory adjustments during physical activity
Baroreflex (BR): Regulates blood pressure and cardiovascular homeostasis
Central Command Neurons: Provide feedforward signals from higher brain centers
Insulin Signaling Insights
Insulin receptors in the nucleus tractus solitarius (NTS) play a critical role in modulating cardiovascular responses
Potential for non-invasive insulin delivery to normalize exercise responses in patients with insulin resistance
3. Sympathetic Nerve Activity and Performance Variability
Microneurographic recordings have unveiled fascinating aspects of muscle sympathetic nerve activity (MSNA):
Significant inter-individual variability in sympathetic discharge patterns
Complex relationships between nerve activity, blood pressure, and exercise responses
Potential for individualized understanding of physiological mechanisms
4. Neural Feedback and Exercise Physiology
The exercise pressor reflex provides critical insights into how muscles communicate with the cardiovascular system:
Activation of group III and IV sensory neurons during muscle contraction
Reflexive modulation of parasympathetic and sympathetic nervous system activity
Potential abnormalities in conditions like heart failure
5. Sleep Deprivation and Exercise Performance
Emerging research demonstrates the intricate relationship between sleep, autonomic function, and exercise:
Physiological Impacts of Sleep Deprivation
Increased sympathetic nervous activity
Decreased parasympathetic activity
Heightened inflammation
Impaired cardiovascular function
Exercise as a Potential Intervention
Regular exercise may mitigate adverse effects of sleep deprivation
Careful management of exercise intensity during sleep-deprived states
6. Vagus Nerve Stimulation: A Breakthrough in Performance Enhancement
A groundbreaking study explored transcutaneous vagus nerve stimulation (tVNS):
Key Findings
Increased peak oxygen consumption (VO2peak) by 1.04 mL/kg/min
Enhanced work rate by 6 watts
Improved heart rate and respiratory rate
Reduced inflammatory response
Clinical Implications:
Autonomic Nervous System Biomarkers: Heart Rate Variability (HRV) emerges as a predictive diagnostic tool for assessing overall physiological readiness, providing a non-invasive window into the body's adaptive capabilities and stress response mechanisms.
Neurometabolic Interactions: The intricate relationship between insulin signaling and cardiovascular responses highlights potential therapeutic interventions for metabolic disorders, suggesting that neural modulation could be a promising approach for managing exercise-related physiological adaptations.
Performance Optimization Strategies: Neural Plasticity research indicates that targeted interventions, such as transcutaneous vagus nerve stimulation, can potentially enhance cardiorespiratory fitness by approximately 1-2%, offering a scientifically validated method for performance enhancement.
Inflammatory Response Management: Evidence demonstrates a direct correlation between autonomic regulation and systemic inflammation, suggesting that comprehensive monitoring of neural activity could provide early indicators of potential health risks and recovery potential.
Sleep-Performance Nexus: The profound impact of sleep deprivation on sympathetic nervous system activity underscores the critical importance of recovery protocols, emphasizing that optimal performance is fundamentally linked to comprehensive physiological restoration.
Individual Variability Considerations: Microneurographic studies reveal significant inter-individual neurological variations, highlighting the necessity for personalized approaches in sports science, rehabilitation, and performance optimization.
Integrated Health Monitoring: The multifaceted research demonstrates that cardiovascular neural control is not simply a binary system but a complex, dynamic network that requires holistic assessment across multiple physiological domains.
Frequently Asked Questions (FAQs)
Q1: What is Heart Rate Variability (HRV)?
HRV measures the variation in time between consecutive heartbeats, reflecting the autonomic nervous system's adaptability and health.
Q2: How Can Athletes Use These Insights?
Monitor HRV as a performance and recovery indicator
Implement targeted training strategies
Pay attention to sleep quality and recovery
Q3: Are These Findings Applicable to All Athletes?
While research provides general insights, individual variations exist. Personalized assessment is recommended.
Key Takeaways
Autonomic nervous system function is critical for athletic performance
HRV provides comprehensive insights beyond traditional metrics
Sleep, neural signaling, and exercise are intricately connected
Individualized approaches yield
the best performance outcomes
Call to Action
Want to Optimize Your Performance?
Consult sports science professionals
Implement HRV monitoring
Prioritize comprehensive recovery strategies
Stay informed about cutting-edge research
Conclusion
In conclusion, the autonomic nervous system (ANS) stands as a critical regulator of exercise performance and overall health. Research underscores the profound impact of exercise training on ANS function, highlighting improvements in cardiovascular, metabolic, and immune responses. Heart rate variability (HRV) emerges as a powerful, non-invasive tool for assessing physiological readiness and guiding personalized training strategies.
The intricate interplay between neural control mechanisms, hormonal signaling, and exercise responses reveals the complexity of human physiology. Emerging interventions, such as transcutaneous vagus nerve stimulation (tVNS), demonstrate the potential to enhance performance and mitigate inflammation. Recognizing the significance of sleep, individual variability, and integrated health monitoring is crucial for optimizing athletic potential and promoting well-being.
Ultimately, understanding the ANS's role in exercise physiology empowers athletes and healthcare professionals to adopt evidence-based strategies, fostering optimal performance and lifelong health. This knowledge paves the way for a future where personalized interventions and comprehensive monitoring revolutionize athletic training and healthcare practices.
Related Articles
Why HIIT is the Best Exercise to Slow Aging and Dramatically Transform Your Body
References
Iannetta, D., Laginestra, F. G., Wray, D. W., & Amann, M. (2025). Dissecting the exercise pressor reflex in heart failure: A multi-step failure. Autonomic Neuroscience, 259, 103269. https://doi.org/10.1016/j.autneu.2025.103269
Tekin, R.T., Kudas, S., Buran, M.M. et al. The relationship between resting heart rate variability and sportive performance, sleep and body awareness in soccer players. BMC Sports Sci Med Rehabil 17, 58 (2025). https://doi.org/10.1186/s13102-025-01093-7
Saputro, R. E., Chou, C. C., Lin, Y. Y., Tarumi, T., & Liao, Y. H. (2025). Exercise-mediated modulation of autonomic nervous system and inflammatory response in sleep-deprived individuals: A narrative reviews of implications for cardiovascular health. Autonomic neuroscience : basic & clinical, 259, 103256. Advance online publication. https://doi.org/10.1016/j.autneu.2025.103256
Teixeira, A. L., & Millar, P. J. (2025). Inter-individual variability in muscle sympathetic nerve activity at rest and during exercise: Disconnection with blood pressure. Autonomic Neuroscience, 258, 103250. https://doi.org/10.1016/j.autneu.2025.103250
Ackland, G. L., Patel, A. B. U., Miller, S., Gutierrez Del Arroyo, A., Thirugnanasambanthar, J., Ravindran, J. I., Schroth, J., Boot, J., Caton, L., Mein, C. A., Abbott, T. E. F., & Gourine, A. V. (2025). Non-invasive vagus nerve stimulation and exercise capacity in healthy volunteers: a randomized trial. European heart journal, ehaf037. Advance online publication. https://doi.org/10.1093/eurheartj/ehaf037
Shanks, J., & Ramchandra, R. (2025). Cardiac Vagal Nerve Activity During Exercise: New insights and future directions. Autonomic Neuroscience, 258, 103254. https://doi.org/10.1016/j.autneu.2025.103254
Daniela, M., Catalina, L., Ilie, O., Paula, M., Daniel-Andrei, I., & Ioana, B. (2022). Effects of Exercise Training on the Autonomic Nervous System with a Focus on Anti-Inflammatory and Antioxidants Effects. Antioxidants, 11(2), 350. https://doi.org/10.3390/antiox11020350
Medical Disclaimer
The information on this website is for informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health care provider with any questions you may have regarding a medical condition or treatment. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
About the Author:
Dr.T.S. Didwal, MD, is an experienced Internal Medicine Physician with over 30 years of practice. Specializing in internal medicine, he is dedicated to promoting wellness, preventive health, and fitness as core components of patient care. Dr. Didwal’s approach emphasizes the importance of proactive health management, encouraging patients to adopt healthy lifestyles, focus on fitness, and prioritize preventive measures. His expertise includes early detection and treatment of diseases, with a particular focus on preventing chronic conditions before they develop. Through personalized care, he helps patients understand the importance of regular health screenings, proper nutrition, exercise, and stress management in maintaining overall well-being.
