The Complex Web of Obesity-Associated Comorbidities: A Comprehensive Overview
Discover the hidden dangers of obesity. This comprehensive overview explores the 224 distinct comorbidities associated with obesity, including cardiovascular disease, diabetes, mental health issues, and more. Learn about the underlying mechanisms and the importance of a holistic approach to obesity management.
DR ANITA JAMWAL MS
9/25/20247 min read
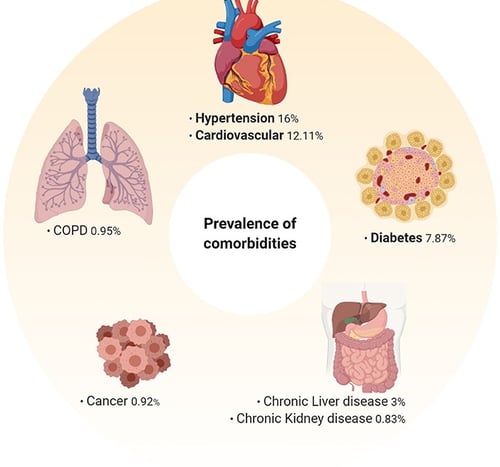
The Review in Gastroenterology Clinics of North America provides a comprehensive overview of the complex network of health issues associated with obesity. It explores the various comorbidities affecting different organ systems, including cardiovascular, endocrine, respiratory, gastrointestinal, musculoskeletal, reproductive, mental health, and cancer. The post delves into the underlying mechanisms, such as inflammation, mechanical effects, metabolic dysregulation, hormonal imbalances, and altered brain function, that contribute to these comorbidities. It emphasizes the importance of a holistic and multidisciplinary approach to obesity management, including personalized treatment plans, patient education, long-term follow-up, and prevention strategies. The conclusion highlights the need for continued research and collaborative efforts to address this significant public health issue.
Key points
Obesity is a complex health condition associated with a wide range of comorbidities affecting various organ systems.
Cardiovascular health is significantly impacted by obesity, leading to conditions like hypertension, coronary artery disease, and heart failure.
Endocrine disorders such as type 2 diabetes, polycystic ovary syndrome, and thyroid dysfunction are commonly linked to obesity.
Respiratory problems including sleep apnea, asthma exacerbations, and obesity hypoventilation syndrome can be exacerbated by obesity.
Gastrointestinal issues like GERD, nonalcoholic fatty liver disease, and gallbladder disease are more prevalent in individuals with obesity.
Musculoskeletal problems such as osteoarthritis, chronic back pain, and increased risk of fractures are associated with obesity.
Mental health can be significantly affected by obesity, leading to depression, anxiety, and low self-esteem.
More Than Just Weight: The Complexities of Obesity
Obesity has become a global health crisis, affecting millions of people worldwide. While the visible effects of excess weight are apparent, what's often overlooked is the intricate network of health issues that accompany obesity. Recent research has uncovered a staggering 224 distinct comorbidities associated with obesity, spanning across multiple medical specialties. This blog post aims to explore the far-reaching impact of obesity on human health, delving into the underlying mechanisms and highlighting the importance of comprehensive care for individuals struggling with obesity.
The Spectrum of Obesity-Associated Comorbidities:
1. Cardiovascular System:
Obesity significantly impacts heart health. Excess weight puts additional strain on the heart, leading to conditions such as:
Hypertension (high blood pressure)
Coronary artery disease
Heart failure
Atrial fibrillation
Deep vein thrombosis
The link between obesity and cardiovascular disease is multifaceted, involving inflammation, metabolic changes, and mechanical stress on the heart and blood vessels.
2. Endocrine System:
Obesity disrupts the delicate balance of hormones in the body, leading to various endocrine disorders:
Type 2 diabetes mellitus
Insulin resistance
Polycystic ovary syndrome (PCOS)
Thyroid dysfunction
Metabolic syndrome
The excess adipose tissue acts as an endocrine organ, secreting hormones and cytokines that interfere with normal metabolic processes.
3. Respiratory System:
Excess weight can compromise lung function and breathing, resulting in:
Obstructive sleep apnea
Asthma exacerbations
Obesity hypoventilation syndrome
Increased risk of respiratory infections
The mechanical load of excess fat on the chest wall and diaphragm, combined with inflammatory processes, contributes to these respiratory issues.
4. Gastrointestinal System:
Obesity affects digestive health in numerous ways:
Gastroesophageal reflux disease (GERD)
Nonalcoholic fatty liver disease (NAFLD)
Gallbladder disease
Increased risk of certain gastrointestinal cancers
The accumulation of visceral fat and alterations in gut microbiota play crucial roles in these digestive complications.
5. Musculoskeletal System:
The extra weight places significant stress on joints and bones:
Osteoarthritis, particularly in weight-bearing joints
Chronic low back pain
Increased risk of fractures
Gout
The combination of mechanical stress and inflammatory processes contributes to these musculoskeletal issues.
6. Reproductive Health:
Obesity can impact fertility and pregnancy:
Reduced fertility in both men and women
Complications during pregnancy (e.g., gestational diabetes, preeclampsia)
Increased risk of birth defects
Menstrual irregularities
Hormonal imbalances and metabolic disturbances associated with obesity underlie these reproductive health issues.
7. Mental Health:
The psychological impact of obesity is significant:
Depression
Anxiety disorders
Low self-esteem
Eating disorders
The relationship between obesity and mental health is complex, involving both physiological and social factors.
8. Cancer Risk:
Obesity is associated with an increased risk of several types of cancer:
Breast cancer (postmenopausal)
Colorectal cancer
Endometrial cancer
Kidney cancer
Esophageal cancer
Chronic inflammation, hormonal imbalances, and metabolic disturbances contribute to the increased cancer risk in individuals with obesity.
Mechanisms Underlying Obesity-Associated Comorbidities:
Inflammation and oxidative Stress:
Chronic low-grade inflammation is a hallmark of obesity. Adipose tissue, once considered merely a storage depot for excess energy, is now recognized as an active endocrine organ. In obesity, adipose tissue undergoes significant changes:
Increased production of pro-inflammatory cytokines: tumor necrosis factor-alpha (TNF-α) and interleukin-6 (IL-6) are key players in this inflammatory cascade. Studies have shown elevated TNF-α mRNA expression in fat biopsy samples from individuals with obesity.
Leptin resistance: Leptin, the "satiety hormone," is produced by adipose tissue. In obesity, despite high levels of leptin, the body becomes resistant to its effects, leading to a dysregulation of appetite and metabolism.
Reduced adiponectin: This anti-inflammatory adipokine is decreased in obesity, further contributing to the pro-inflammatory state.
The chronic inflammation associated with obesity creates a state of oxidative stress, damaging cellular structures and contributing to the development of various comorbidities.
Mechanical Effects:
The physical burden of excess weight has two primary effects:
Direct loading: The extra weight places stress on weight-bearing joints, contributing to conditions like osteoarthritis and chronic back pain.
Ectopic fat distribution: Fat can accumulate in organs not typically associated with fat storage, such as the liver, heart, and pancreas. This ectopic fat distribution can lead to organ dysfunction and contribute to conditions like nonalcoholic fatty liver disease and cardiovascular complications.
Renin-Angiotensin-Aldosterone System (RAAS) and Sympathetic Nervous System (SNS) activation:
Obesity is associated with increased activity of both the RAAS and SNS:
RAAS activation: This leads to increased sodium retention and blood volume expansion, contributing to hypertension.
SNS activation: Increased sympathetic activity raises heart rate and blood pressure, further exacerbating hypertension and cardiovascular risk.
These changes in the RAAS and SNS, combined with altered diuresis and natriuresis patterns, create a perfect storm for the development of hypertension in obesity.
Metabolic Dysregulation:
Obesity profoundly affects metabolism:
Insulin resistance: As adipose tissue expands, it becomes less responsive to insulin, leading to elevated blood glucose levels and, eventually, type 2 diabetes.
Dyslipidemia: Obesity is associated with abnormal lipid profiles, including elevated triglycerides and low HDL cholesterol, contributing to cardiovascular risk.
Altered glucose metabolism: impaired glucose tolerance and increased hepatic glucose production further contribute to the development of diabetes.
Hormonal Imbalances:
Obesity disrupts the delicate balance of hormones in the body:
Sex hormones: In men, obesity can lead to decreased testosterone levels. In women, it can cause menstrual irregularities and contribute to polycystic ovary syndrome (PCOS).
Cortisol: Chronic stress associated with obesity can lead to dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis, affecting cortisol levels and contributing to metabolic disturbances.
Altered Brain Structure and Function:
Emerging research suggests that obesity can impact brain structure and function:
Changes in reward circuitry: Obesity may alter the brain's reward system, affecting appetite regulation and food-seeking behavior.
Cognitive function: Some studies have linked obesity to an increased risk of cognitive decline and dementia in later life.
Impaired Immunity:
Obesity can compromise immune function:
Altered immune responses: Obesity is associated with changes in both innate and adaptive immunity, potentially increasing susceptibility to infections.
Chronic inflammation: The pro-inflammatory state in obesity can lead to a dysregulated immune response.
Other Mechanisms:
Several other mechanisms contribute to the development of obesity-associated comorbidities:
Increased uric acid production: contributing to the development of gout and kidney stones.
Microbiome alterations: Changes in gut bacteria composition may influence metabolism and inflammation.
Mechanical obstruction: In severe obesity, physical obstruction of airways can contribute to sleep apnea.
Implications for Clinical Practice:
The vast array of obesity-associated comorbidities highlights the need for a comprehensive approach to obesity management:
Holistic Assessment:
Clinicians should conduct thorough evaluations of patients with obesity, screening for potential comorbidities across multiple organ systems. This may include:
Cardiovascular risk assessment
Metabolic panel including lipid profile and glucose tolerance testing
Sleep studies to evaluate for sleep apnea
Mental health screening
Regular cancer screenings as appropriate
Multidisciplinary Care:
Given the complexity of obesity and its associated comorbidities, a multidisciplinary approach is often necessary. This may involve collaboration between:
Primary care physicians
Endocrinologists
Cardiologists
Pulmonologists
Orthopedic specialists
Mental health professionals
Nutritionists and dietitians
Personalized Treatment Plans:
Treatment should be tailored to the individual, addressing both weight management and specific comorbidities. This may include:
Lifestyle interventions (diet and exercise)
Pharmacological treatments
Bariatric surgery in appropriate cases
Management of specific comorbidities (e.g., diabetes medications, antihypertensives)
Patient Education:
Educating patients about the health risks associated with obesity and the benefits of weight loss is crucial. This can improve motivation and adherence to treatment plans.
Long-term Follow-up:
Given the chronic nature of obesity and its comorbidities, long-term follow-up and support are essential for successful management.
Prevention Strategies:
Implementing strategies to prevent obesity, especially in high-risk populations, is crucial for public health. This may include:
Early education on healthy lifestyle habits
Policy changes to promote healthier food environments
Community-based interventions to increase physical activity
Conclusion:
The complex web of obesity-associated comorbidities underscores the far-reaching impact of excess weight on human health. From cardiovascular disease to mental health issues, obesity affects nearly every aspect of well-being. Understanding the underlying mechanisms, from chronic inflammation to mechanical stress, provides insights into potential treatment targets and the importance of comprehensive care.
As our understanding of obesity and its associated comorbidities continues to evolve, so too must our approach to treatment and prevention. By addressing obesity as a chronic disease with multiple facets, we can work towards more effective interventions and improved outcomes for individuals struggling with this condition.
The challenge of obesity and its associated comorbidities is significant, but with continued research, collaborative care, and a focus on both treatment and prevention, we can make strides in improving health outcomes for millions of people worldwide. As healthcare providers, policymakers, and individuals, we all have a role to play in addressing this critical public health issue.
Related Articles:
1.The Role of Obesity Medications in Maintaining Muscle During Weight Loss
2.Understanding the Science Behind Body Weight and Metabolism: Your Key to Sustainable Weight Loss
Journal Reference
Yuen, M. M. (2023). Health Complications of Obesity: 224 Obesity-Associated Comorbidities from a Mechanistic Perspective. Gastroenterology Clinics of North America, 52(2), 363-380. https://doi.org/10.1016/j.gtc.2023.03.006
Image credit: https://www.frontiersin.org/files/Articles/567283/fimmu-11-01991-HTML-r1/image_m/fimmu-11-01991-g003.jpg
Disclaimer
