The Lipotoxicity Effect: How Fat Infiltration Can Harm Your Bones and Muscles
Fatty infiltration is a serious condition where excess fat accumulates in bones and muscles. This can lead to osteoporosis, sarcopenia, and insulin resistance. Learn about the causes, effects, and potential treatments for fatty infiltration in this informative article.
DR TS DIDWAL MS
9/15/20249 min read
Fatty infiltration in the musculoskeletal system is a silent threat that occurs when excess fat accumulates in bones and muscles. This abnormal accumulation can lead to serious health problems, including osteoporosis, sarcopenia, and insulin resistance. Age, obesity, inflammation, and glucocorticoids are common risk factors. While imaging techniques like MRI and CT can help diagnose fatty infiltration, lifestyle changes, targeted therapies, and medical interventions offer potential solutions. By understanding and addressing this condition, we can improve musculoskeletal health and overall quality of life.
Key Points
Fatty infiltration is when excess fat accumulates in bones and muscles, causing problems.
It can lead to weak bones, weak muscles, and difficulty controlling blood sugar.
Common risk factors include getting older, being overweight, having inflammation, and taking certain medications.
Imaging tests can help doctors see fatty infiltration.
Lifestyle changes, targeted treatments, and medical interventions can help address it.
Maintaining a healthy balance between bone, muscle, and fat is important for overall health.
Addressing fatty infiltration can improve bone health, muscle strength, and overall well-being.
Fatty Infiltration in the Musculoskeletal System: A Silent Threat
As we age, our bodies undergo numerous changes, some visible and others hidden beneath the surface. One such change that's been gaining attention in the medical community is fatty infiltration in the musculoskeletal system. But what exactly is this phenomenon, and why should we care? Let's embark on a journey through the intricate world of bones, muscles, and fat to uncover the secrets of this silent threat.
The Musculoskeletal System: More Than Just Bones and Muscles
Before we dive into fatty infiltration, let's take a moment to appreciate the marvel that is our musculoskeletal system. This complex network of bones, muscles, ligaments, tendons, and cartilage isn't just responsible for keeping us upright and mobile. It's also a crucial player in our endocrine and immune functions. Think of it as the body's scaffolding, engine, and defense system all rolled into one!
Fatty Infiltration: The Uninvited Guest
Now, imagine this well-oiled machine slowly being infiltrated by tiny droplets of fat. That's essentially what fatty infiltration is - the abnormal accumulation of adipocytes (fat cells) in tissues where they don't belong. It's like finding oil drops in your car's coolant system - it's not supposed to be there, and it can cause some serious problems.
Types of Adipose Tissue: Not All Fat is Created Equal
Before we vilify all fat, it's important to understand that not all adipose tissue is created equal. There are three main types:
White Adipose Tissue (WAT): The storage unit of our body, WAT is what we typically think of as "fat."
Brown Adipose Tissue (BAT): This metabolically active fat helps regulate body temperature.
Beige Adipose Tissue: A hybrid of WAT and BAT, it can switch between energy storage and burning.
In the context of fatty infiltration, it's primarily WAT that we're concerned about. But interestingly, recent research suggests that promoting the "browning" of white fat could be a potential therapeutic strategy. More on that later!
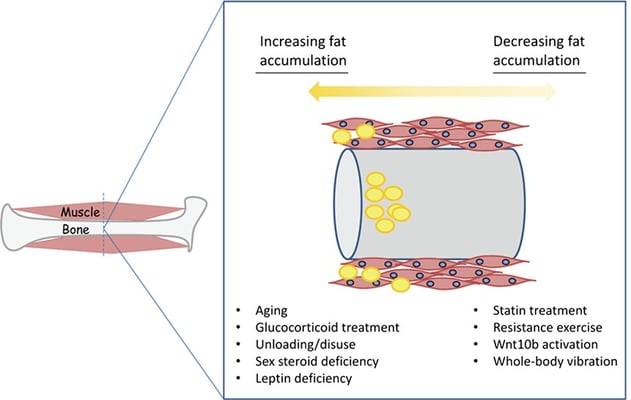
The Bone-Muscle-Fat Triangle: A Delicate Balance
The relationship between bone, muscle, and fat is like a complex dance. They all originate from the same type of stem cells, which means changes in one can have ripple effects on the others. This interconnectedness is why fatty infiltration is such a fascinating and important area of study.
Bone: The Foundation Under Siege
In healthy bones, there's a delicate balance between bone formation (osteoblasts) and bone resorption (osteoclasts). Fatty infiltration throws a wrench in this process:
It inhibits the formation of new bone cells
It enhances bone resorption
It can lead to lipoapoptosis (cell death) of bone cells
The result? A higher risk of osteoporosis and fractures. It's like termites slowly weakening the foundation of a house.
Muscle: Strength Sapped by Fat
Muscles aren't immune to fatty infiltration either. As fat accumulates within and between muscle fibers, it can:
Impair muscle fiber regeneration
Reduce muscle strength and function
Contribute to insulin resistance
This process is particularly problematic in conditions like sarcopenia, where muscle mass and strength decrease with age.
The Culprits Behind Fatty Infiltration
So, what causes this fatty invasion? Several factors come into play:
Aging: As we get older, our bodies's ability to regulate fat distribution declines.
Obesity: Excess body fat can spill over into non-adipose tissues.
Inflammation: Chronic inflammation can disrupt normal tissue function and promote fatty infiltration.
Glucocorticoid Use: Long-term use of these medications can alter fat distribution.
Clinical Implications: When Fatty Infiltration Becomes Problematic
The effects of fatty infiltration aren't just theoretical; they manifest in real clinical conditions:
Osteoporosis: Bones Weakened by Fat
Osteoporosis, characterized by reduced bone mass and increased fracture risk, has a strong link to fatty infiltration. Studies have shown a negative correlation between bone mineral density and marrow adipose tissue. In other words, as fat in the bone marrow increases, bone density decreases.
Sarcopenia: Muscles Losing the Battle to Fat
Sarcopenia, the age-related loss of muscle mass and strength, is exacerbated by fatty infiltration. As fat replaces muscle tissue, it creates a vicious cycle of reduced physical function and increased risk of further fat accumulation.
Osteosarcopenic Obesity: The Perfect Storm
When osteoporosis, sarcopenia, and obesity converge, we get a condition called osteosarcopenic obesity. It's like a perfect storm of musculoskeletal deterioration, highlighting the interconnected nature of bone, muscle, and fat health.
Diagnosing Fatty Infiltration: Seeing the Unseen
One of the challenges with fatty infiltration is that it's not visible to the naked eye. Thankfully, modern imaging techniques have come to the rescue:
Magnetic Resonance Imaging (MRI): Can provide detailed images of fat distribution in tissues.
Computed Tomography (CT): Useful for assessing bone density and fat content.
Dual-Energy X-ray Absorptiometry (DEXA): Primarily used for bone density but can also estimate body composition.
Lipotoxicity Effect: When Fat Turns Toxic
At the cellular level, fatty infiltration isn't just about space occupation. The excess fat can produce toxic substances that wreak havoc on surrounding tissues. This phenomenon, known as lipotoxicity, can:
Trigger inflammation
Cause oxidative stress
Lead to cell death
It's like having a toxic waste dump in the middle of a thriving ecosystem - nothing good can come of it.
Fighting Back: Potential Therapeutic Approaches
While fatty infiltration presents a significant challenge, researchers and clinicians are exploring various strategies to combat this issue. Let's delve deeper into these promising approaches:
1. Inducing Adipose Browning: Turning Bad Fat Good
One of the most exciting avenues of research involves transforming harmful white adipose tissue (WAT) into more metabolically active brown adipose tissue (BAT) or beige adipose tissue. This process, known as "browning," could help mitigate the negative effects of fatty infiltration.
How it works:
BAT and beige fat are more metabolically active, burning energy rather than storing it.
Browning can increase energy expenditure and improve metabolic health.
Potential methods:
Cold exposure: Controlled exposure to cold temperatures can stimulate browning.
Exercise: Certain types of exercise, particularly resistance training, may promote browning.
Pharmacological agents: Drugs that activate β3-adrenergic receptors or PPAR-γ coactivator 1-α (PGC-1α) are being investigated.
Challenges:
Ensuring targeted browning without affecting necessary WAT stores.
Developing safe and effective methods for long-term browning induction.
2. Targeting Specific Molecules: Precision Medicine Approach
Several molecular targets have shown promise in combating fatty infiltration and its effects:
a) mTOR Inhibition
mTOR (mammalian target of rapamycin) is a key regulator of cell metabolism and growth.
Rapamycin, an mTOR inhibitor, has shown potential in reducing lipoapoptosis (cell death due to lipotoxicity).
How it works: Inhibiting mTOR can help maintain osteoblast viability and reduce the harmful effects of palmitic acid, a common saturated fatty acid.
Challenges: Balancing mTOR inhibition to prevent fatty infiltration without disrupting normal cell growth and function.
b) Liver X Receptor (LXR) Activation
LXRs are nuclear receptors that play crucial roles in lipid metabolism and inflammation.
3. Lifestyle Interventions: The Power of Healthy Habits
Never underestimate the impact of lifestyle changes in combating fatty infiltration:
a) Exercise
High-intensity endurance training has shown particular promise in preventing muscle fatty infiltration, especially in elderly individuals with early-stage sarcopenia.
Resistance training can help maintain and build muscle mass, potentially offsetting fatty infiltration.
How it works:
Increases muscle insulin sensitivity
Promotes muscle protein synthesis
Enhances mitochondrial function
Stimulates myokine production, which can have anti-inflammatory effects
b) Diet
A balanced, anti-inflammatory diet may help combat fatty infiltration:
Mediterranean diet: Rich in fruits, vegetables, whole grains, and healthy fats
Omega-3 fatty acids: Found in fish, flaxseeds, and walnuts, can help reduce inflammation
Antioxidant-rich foods: Berries, leafy greens, and nuts can combat oxidative stress
Adequate protein intake: Essential for maintaining muscle mass and bone health
c) Stress Management
Chronic stress can contribute to inflammation and metabolic disruption, potentially exacerbating fatty infiltration.
Stress-reduction techniques:
Mindfulness meditation
Yoga
Regular sleep habits
Social connections and support
4. Pharmacological Approaches: Medical Interventions
Several drugs are being investigated for their potential in combating fatty infiltration:
a) Statins
Primarily known for lowering cholesterol, statins may also help improve bone mineral density.
Mechanism: Statins inhibit the expression of lipoprotein lipase and PPAR-γ2, potentially reducing fatty infiltration in bone marrow.
Considerations: The effects of statins on bone health appear to be dose-dependent, requiring careful dosage optimization.
b) N-acetylcysteine (NAC)
A powerful antioxidant that could help combat oxidative stress associated with fatty infiltration.
Potential benefits:
Reduction of inflammation
Protection against lipotoxicity
Support of glutathione production, a key cellular antioxidant
c) Vitamin D
Essential for both bone and muscle health, vitamin D deficiency is associated with increased fatty infiltration.
Supplementation may help:
Improve calcium absorption for bone health
Enhance muscle function and reduce fall risk
Modulate inflammation and immune function
d) Resveratrol
A compound found in red wine and some berries, resveratrol, has shown promise in animal studies.
Potential mechanisms:
Activation of SIRT1, a protein involved in cellular metabolism and aging
Anti-inflammatory and antioxidant effects
Promotion of brown adipose tissue activity
e) Emerging Therapies
PTH (Parathyroid Hormone) and risedronate: Commonly used in osteoporosis treatment, these drugs have shown inhibitory effects on intramedullary adiposity while regulating bone homeostasis.
SLN (Sarcolipin) expression enhancers: Increasing sarcolipin expression may help combat fatty infiltration in muscle tissue.
5. Combination Approaches: The Power of Synergy
Given the complex nature of fatty infiltration, combination therapies that target multiple aspects of the condition may prove most effective. For example:
Lifestyle interventions (exercise and diet) combined with pharmacological treatments
Browning induction therapies alongside molecular targeting approaches
Personalized treatment plans based on individual patient characteristics and the specific patterns of fatty infiltration
As research progresses, these combination approaches may offer the most promising path forward in treating fatty infiltration and its associated musculoskeletal conditions.
The Road Ahead: Challenges and Opportunities
While we've made significant strides in understanding fatty infiltration, many questions remain:
How can we develop stable musculoskeletal fatty infiltration models for research?
Are other components of the musculoskeletal system (tendons, ligaments, cartilage) affected by lipotoxicity?
How do we quantify fatty infiltration accurately for clinical diagnosis?
Can we develop targeted therapies that address fatty infiltration without causing unwanted side effects?
These questions represent both challenges and exciting opportunities for future research.
Conclusion: A Call to Action
Fatty infiltration in the musculoskeletal system is more than just an interesting scientific phenomenon—it's a critical health issue that affects millions of people, particularly as our global population ages. By understanding the mechanisms behind fatty infiltration, we can develop better strategies for prevention and treatment.
As we continue to unravel the mysteries of the bone-muscle-fat relationship, one thing is clear: maintaining a healthy balance is key. Whether through lifestyle changes, medical interventions, or a combination of both, taking steps to combat fatty infiltration can have profound effects on our musculoskeletal health and overall quality of life.
So the next time you think about your health, remember it's not just about what's on the outside. The hidden dance of fat, muscle, and bone within your body plays a crucial role in keeping you strong, mobile, and healthy for years to come. Let's give our musculoskeletal system the attention and care it deserves!
Faqs
Q: How does lipotoxicity affect the body?
A: Lipotoxicity is a condition where excess lipids accumulate in non-adipose tissues, leading to cellular dysfunction and death. This can cause various health problems, including:
Lipotoxicity as a therapeutic target in obesity and diabetic cardiomyopathy
Insulin resistance: Difficulty in regulating blood sugar levels.
Type 2 diabetes: A chronic condition characterized by high blood sugar levels.
Cardiovascular disease: Heart disease, stroke, and other conditions related to the heart and blood vessels.
Fatty liver disease: Excessive fat accumulation in the liver.
Inflammation: Chronic inflammation throughout the body.
Q: Is lipotoxicity a systemic or local disease?
A: Lipotoxicity is a systemic disease, meaning it affects multiple organs and tissues throughout the body. While it can initially manifest in specific areas, such as the liver or pancreas, its effects can spread and impact overall health.
Q: How do lipotoxic lipids affect vascular function?
A: Lipotoxic lipids can negatively impact vascular function in several ways:
Endothelial dysfunction: Damage to the inner lining of blood vessels, leading to increased risk of blood clots and inflammation.
Atherosclerosis: buildup of plaque in the arteries, which can lead to heart attacks and strokes.
Increased blood pressure: High blood pressure can strain the heart and blood vessels.
Inflammation: Chronic inflammation can contribute to vascular damage and disease.
Related Articles:
How to Lose Weight Without Losing Muscle : Lean Muscle Building and Fat Loss
Journal Reference :
Zhu, Y., Hu, Y., Pan, Y., Li, M., Niu, Y., Zhang, T., Sun, H., Zhou, S., Liu, M., Zhang, Y., Wu, C., Ma, Y., Guo, Y., & Wang, L. (2024). Fatty infiltration in the musculoskeletal system: Pathological mechanisms and clinical implications. Frontiers in Endocrinology, 15, 1406046. https://doi.org/10.3389/fendo.2024.1406046
Image credit: http://www.frontiersin.org/files/Articles/208170/fendo-07-00069-HTML/image_m/fendo-07-00069-g002.jpg
Disclaimer
The information on this website is for informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health care provider with any questions you may have regarding a medical condition or treatment. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. This blog post is based on current scientific understanding and research. Always consult with healthcare professionals for personalized medical advice.
