Visceral Fat, Adiposity, and Cardiometabolic Diseases in Asians: Insights from the HELIOS Study
Uncover the hidden dangers of visceral fat in Asian populations. Learn how excess adiposity contributes to cardiometabolic diseases like diabetes and heart disease. Discover the latest insights from the HELIOS Study and explore strategies for prevention and management
DR T S DIDWAL MD
8/30/20247 min read
The HELIOS Study, published in The Lancet Diabetes & Endocrinology, conducted in Singapore, investigated the relationship between adiposity, ethnicity, and cardiometabolic health among Asian populations. The study found significant ethnic disparities in obesity, type 2 diabetes, and other cardiometabolic diseases, with Malay and Indian participants at higher risk compared to Chinese participants. Visceral fat was identified as a key risk factor, but additional mechanisms were also implicated. The study highlights the need for ethnicity-specific approaches to the prevention and treatment of cardiometabolic diseases in Asian populations.
Key points
Ethnic Disparities: The study clearly demonstrates marked differences in cardiometabolic risk profiles among various Asian ethnic groups, emphasizing the need for ethnicity-specific approaches to prevention and treatment.
Visceral Adiposity: The study reinforces the critical role of visceral fat as an independent risk factor for metabolic disease across Asian populations, highlighting its importance in targeted interventions.
Beyond Adiposity: The findings challenge the sole reliance on adiposity-based explanations for ethnic disparities, suggesting the involvement of additional mechanisms that require further investigation.
Implications for Clinical Practice: The study provides valuable insights for healthcare professionals, emphasizing the need for more nuanced risk assessment tools, personalized approaches, and a focus on visceral adiposity management.
Research Directions: The study opens new avenues for research, including the exploration of non-adiposity-related factors, genetic and epigenetic influences, and the development of more effective intervention strategies.
The Rising Tide of Cardiometabolic Diseases in Asia: Insights from the HELIOS Study
In recent years, the Asia-Pacific region has witnessed a dramatic surge in cardiometabolic diseases, particularly type 2 diabetes and cardiovascular disease. This trend has caught the attention of researchers and healthcare professionals worldwide, prompting investigations into the underlying causes and potential interventions. A groundbreaking study conducted in Singapore, known as the Health for Life in Singapore (HELIOS) Study, has shed new light on this pressing issue, revealing intriguing insights into the complex interplay between adiposity, ethnicity, and cardiometabolic health among Asian populations.
Understanding the HELIOS Study
The HELIOS Study is a comprehensive, population-based cohort study that focuses on multiethnic Asian men and women living in Singapore. With participants ranging from 30 to 84 years old, this study offers a unique opportunity to examine the factors contributing to cardiometabolic diseases across different Asian ethnic subgroups.
Key aspects of the study include:
1. Body composition assessment using dual-energy x-ray absorption
2. Detailed metabolic characterization
3. Analysis of cardiometabolic phenotypes, including glycemic indices, lipid levels, and blood pressure
4. Evaluation of disease outcomes such as type 2 diabetes, hypercholesterolaemia, and hypertension
5. Assessment of metabolic syndrome scores
The study's design allows for a comprehensive examination of the relationship between adiposity (particularly visceral fat) and various cardiometabolic risk factors across different Asian ethnic groups.
Study Participants and Demographics
Between April 2018 and January 2022, the HELIOS study recruited 10,004 individuals, with 9,067 meeting the inclusion criteria for the final analysis. The participant breakdown was as follows:
Gender: 59.6% female (5,404) and 40.4% male (3,663)
Ethnicity: 68.6% Chinese (6,224), 12.9% Malay (1,169), and 18.5% Indian (1,674)
Mean age: 52.8 years (SD 11.8)
This diverse cohort provided researchers with a robust dataset to explore the nuances of cardiometabolic health across different Asian ethnic subgroups.
Prevalence of Cardiometabolic Diseases
The study revealed concerning prevalence rates for several cardiometabolic diseases:
Type 2 diabetes: 8.2% (744 participants)
Hypercholesterolaemia: 27.2% (2,469 participants)
Hypertension: 18.0% (1,630 participants)
These figures underscore the significant burden of cardiometabolic diseases in the Singaporean population and highlight the urgent need for targeted interventions and prevention strategies.
Ethnic Disparities in Cardiometabolic Health
One of the most striking findings of the HELIOS study was the marked disparity in cardiometabolic health profiles among different Asian ethnic groups. Notably, Malay and Indian participants exhibited significantly higher risks for obesity and type 2 diabetes compared to their Chinese counterparts:
1. Obesity and Type 2 Diabetes Risk: Malay and Indian participants had 3-4 times higher odds of obesity and type 2 diabetes than Chinese participants.
2. Adverse Metabolic and Adiposity Profiles: Malay and Indian participants also demonstrated less favorable metabolic and adiposity profiles compared to Chinese participants.
These disparities raise important questions about the underlying factors contributing to increased cardiometabolic risk in certain Asian ethnic subgroups.
The Role of Visceral Adiposity
A key focus of the HELIOS study was the examination of visceral fat mass index (vFMI) and its relationship to cardiometabolic health. The findings revealed that excess adiposity, particularly visceral fat, was strongly associated with adverse cardiometabolic health indices, including an increased risk of type 2 diabetes.
Key observations regarding visceral adiposity include:
1. Independent Risk Factor: Visceral adiposity emerged as an independent risk factor for metabolic disease across all Asian populations studied.
2. Contribution to Type 2 Diabetes: Excess visceral fat accounted for a large fraction of type 2 diabetes cases in each of the ethnic groups examined.
3. Ethnic Differences in Triglycerides and Blood Pressure: Variations in vFMI explained the differences in triglyceride levels and blood pressure observed between the Asian ethnic groups.
These findings underscore the critical role of visceral adiposity in driving cardiometabolic risk and highlight the importance of targeting this specific fat depot in prevention and treatment strategies.
Beyond Adiposity: Uncovering Additional Mechanisms
While visceral adiposity emerged as a significant contributor to cardiometabolic risk, the HELIOS study also revealed that it doesn't tell the whole story. Intriguingly, increased vFMI did not fully explain certain metabolic disparities observed among Indian participants:
1. Higher Glucose Levels: Indian participants exhibited elevated glucose levels that were not entirely accounted for by differences in visceral adiposity.
2. Reduced Insulin Sensitivity: The decreased insulin sensitivity observed in Indian participants was not fully explained by variations in vFMI.
3. Increased Type 2 Diabetes Risk: The heightened risk of type 2 diabetes among Indian participants persisted even after accounting for differences in visceral adiposity.
These findings suggest that additional mechanisms, beyond adiposity alone, play a crucial role in determining cardiometabolic risk among Asian populations, particularly in certain ethnic subgroups.
Implications for Research and Clinical Practice
The insights gained from the HELIOS study have far-reaching implications for both research and clinical practice in the field of cardiometabolic health:
1. Targeted Interventions: The study underscores the need for ethnicity-specific approaches to prevention and treatment of cardiometabolic diseases in Asian populations.
2. Focus on Visceral Adiposity: Healthcare professionals should prioritize the assessment and management of visceral adiposity as a key risk factor for metabolic disease in Asian individuals.
3. Beyond BMI: The findings highlight the limitations of relying solely on BMI as a measure of cardiometabolic risk, emphasizing the importance of more sophisticated body composition assessments.
4. Exploration of Additional Mechanisms: The study opens new avenues for research into the non-adiposity-related factors contributing to cardiometabolic risk in Asian populations, particularly among Indian individuals.
5. Personalized Risk Assessment: The observed ethnic disparities suggest the need for more nuanced, ethnicity-specific risk assessment tools for cardiometabolic diseases in Asian populations.
6. Public Health Strategies: Policymakers and public health officials should consider the ethnic variations in cardiometabolic risk when designing and implementing population-level interventions.
Challenges and Future Directions
While the HELIOS study provides valuable insights, it also highlights several challenges and areas for future research:
1. Longitudinal Studies: To better understand the causal relationships between adiposity, ethnicity, and cardiometabolic risk, long-term follow-up studies are needed.
2. Mechanistic Investigations: Further research is required to elucidate the additional mechanisms contributing to increased cardiometabolic risk in certain Asian ethnic subgroups, particularly among Indian individuals.
3. Intervention Studies: Clinical trials targeting visceral adiposity reduction in Asian populations are needed to evaluate the impact on cardiometabolic outcomes across different ethnic groups.
4. Genetic and Epigenetic Factors: Exploration of genetic and epigenetic variations among Asian ethnic subgroups may provide insights into the observed disparities in cardiometabolic risk.
5. Environmental and Lifestyle Factors: Future studies should investigate the role of environmental and lifestyle factors in modulating the relationship between adiposity and cardiometabolic risk in Asian populations.
6. Translation to Clinical Practice: Developing practical tools and guidelines for assessing and managing visceral adiposity in clinical settings remains a crucial challenge.
Conclusion
The HELIOS study has provided a wealth of information on the complex relationship between adiposity, ethnicity, and cardiometabolic health in Asian populations. By highlighting the significant role of visceral adiposity as an independent risk factor for metabolic disease, while simultaneously revealing the limitations of adiposity-based explanations for ethnic disparities, this study has opened new avenues for research and clinical practice.
As the burden of cardiometabolic diseases continues to grow in the Asia-Pacific region, the insights gained from the HELIOS study offer a foundation for developing more targeted, ethnicity-specific approaches to prevention and treatment. Moving forward, a multifaceted approach that combines adiposity management with exploration of additional risk factors will be crucial in addressing the rising tide of cardiometabolic diseases in Asian populations.
Faqs:
1. What disease is visceral adiposity?
Visceral adiposity is not a disease itself, but it refers to the accumulation of fat around internal organs, particularly in the abdominal area. This type of fat is associated with a higher risk of developing various diseases, including metabolic syndrome, type 2 diabetes, cardiovascular diseases, and certain cancers.
2. What disease is caused by visceral fat?
Visceral fat is linked to several diseases, including type 2 diabetes, cardiovascular diseases (such as coronary artery disease and hypertension), metabolic syndrome, and non-alcoholic fatty liver disease (NAFLD). It also increases the risk of certain types of cancer, including breast and colorectal cancer.
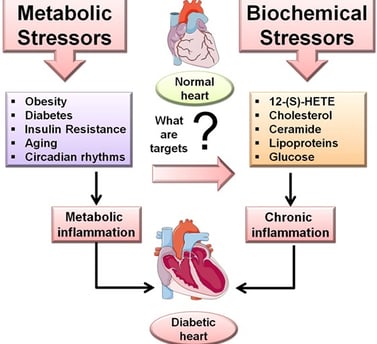
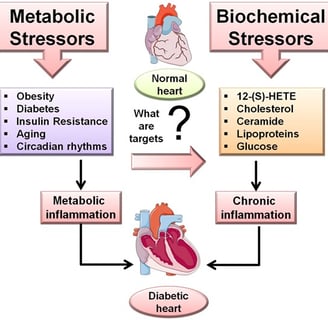
3. What is the relationship between visceral fat and disease development?
Visceral fat is metabolically active and releases inflammatory cytokines, hormones, and free fatty acids that contribute to insulin resistance, inflammation, and dyslipidemia. These factors play a critical role in the development of diseases such as type 2 diabetes, cardiovascular diseases, and metabolic syndrome.
4. How does visceral fat cause cardiovascular disease?
Visceral fat contributes to cardiovascular disease by promoting insulin resistance, systemic inflammation, and dyslipidemia (abnormal lipid levels). These conditions lead to the development of atherosclerosis (hardening of the arteries), hypertension (high blood pressure), and other factors that increase the risk of heart attacks, strokes, and other cardiovascular events.
Journal Reference
Mina, T., Xie, W., Low, D. Y., Wang, X., Lam, B. C. C., Sadhu, N., Ng, H. K., Aziz, N., Tong, T. Y. Y., Kerk, S. K., Choo, W. L., Low, G. L., Ibrahim, H., Lim, L., Tai, E. S., Wansaicheong, G., Dalan, R., Yew, Y. W., Elliott, P., . . . Chambers, J. (2024). Adiposity and metabolic health in Asian populations: An epidemiological study using dual-energy x-ray absorptiometry in Singapore. The Lancet Diabetes & Endocrinology. https://doi.org/10.1016/S2213-8587(24)00195-5
Image credit:https://www.frontiersin.org/files/Articles/258167/fcvm-04-00031-HTML/image_m/fcvm-04-00031-g001.jpg
Related
https://healthnewstrend.com/polycystic-ovary-syndrome-and-type-2-diabetes-whats-the-link
Disclaimer
The information on this website is for informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health care provider with any questions you may have regarding a medical condition or treatment. Never disregard professional medical advice or delay in seeking it because of something you have read on this website
