What is Mild Cognitive Impairment? How to Recognize Early Signs of MCI & Can it be prevented?
Are you concerned about memory loss or cognitive changes? Learn about Mild Cognitive Impairment (MCI) and how to recognize early signs, seek diagnosis, and explore effective treatment options.
DR T S DIDWAL MD
8 min read
According to a review published in Frontiers in Neurology, mild cognitive impairment (MCI) is a transitional stage between normal aging and dementia. It involves noticeable cognitive decline but doesn't significantly interfere with daily life. While not everyone with MCI will develop dementia, it increases the risk. Common symptoms include memory problems, difficulty finding words, and trouble following conversations. Diagnosis involves a medical history review, cognitive tests, and brain scans. Management focuses on lifestyle modifications, medical treatment, cognitive training, and safety planning. There are no FDA-approved medications specifically for MCI, but some treatments may help slow progression. Early detection is crucial for effective intervention and planning.
Key Points
Mild cognitive impairment (MCI) is a transitional stage between normal aging and dementia.
It involves noticeable cognitive decline but doesn't significantly interfere with daily life.
While not everyone with MCI will develop dementia, it increases the risk.
Common symptoms include memory problems, difficulty finding words, and trouble following conversations.
Diagnosis involves medical history review, cognitive tests, and brain scans.
Management focuses on lifestyle modifications, medical treatment, cognitive training, and safety planning.
Early detection is crucial for effective intervention and planning.
Mild Cognitive Impairment: Understanding the Early Stages of Cognitive Decline
Cognitive decline is a concern that weighs heavily on many people's minds as they age. While some changes in memory and thinking skills are a normal part of getting older, more significant declines may signal the early stages of dementia. In recent years, medical experts have focused increasing attention on a condition known as mild cognitive impairment (MCI)—an important transitional stage between normal age-related cognitive changes and more serious dementia.
What is Mild Cognitive Impairment?
Mild cognitive impairment refers to cognitive decline that is greater than expected for a person's age and education level but does not significantly interfere with daily life and activities. People with MCI show noticeable problems with memory, language, thinking, or judgment, but are still able to function independently for the most part. MCI is considered an intermediate stage between the cognitive decline associated with normal aging and the more pronounced deficits seen in dementia. Not everyone with MCI will go on to develop dementia, but it does increase the risk. According to recent studies, about 6–15% of people with MCI progress to Alzheimer's disease each year. The prevalence of MCI among older adults varies in different parts of the world but is estimated to be around 15–25% in most populations studied. As our global population ages, MCI is becoming an increasingly common condition that warrants greater attention from the medical community and public health systems.
Recognizing the Signs of MCI
So how can you tell if cognitive changes are normal aging or potentially MCI? Some key signs and symptoms of MCI include:
Memory problems, especially trouble remembering recent events or conversations
Frequently losing or misplacing items
Forgetting appointments or important dates
Trouble coming up with the right words
Taking longer to complete familiar tasks
Difficulty following the flow of a conversation
Decreased ability to make sound judgments or decisions
Changes in mood or behavior, such as increased anxiety, irritability or apathy
Getting lost in familiar places
Importantly, in MCI, these changes are noticeable to the individual and often to close family/friends, but do not significantly impair the person's ability to carry out daily activities independently. When cognitive deficits begin interfering with a person's ability to function in daily life, this may signal progression to dementia.
Diagnosing Mild Cognitive Impairment
If you or a loved one are experiencing cognitive changes that seem concerning, it's important to consult with a doctor for a proper evaluation. There is no single definitive test for MCI. Instead, diagnosis typically involves a combination of the following:
Medical history and symptoms review
Physical and neurological exam
Cognitive and memory tests
Brain imaging scans like MRI or CT
Blood tests to rule out other causes
Mental health evaluation
The core of MCI diagnosis revolves around cognitive testing. A variety of neuropsychological tests may be used to assess different aspects of thinking and memory. Common screening tests include:
Mini-Mental State Examination (MMSE)
Montreal Cognitive Assessment (MoCA)
Mini-Cog test
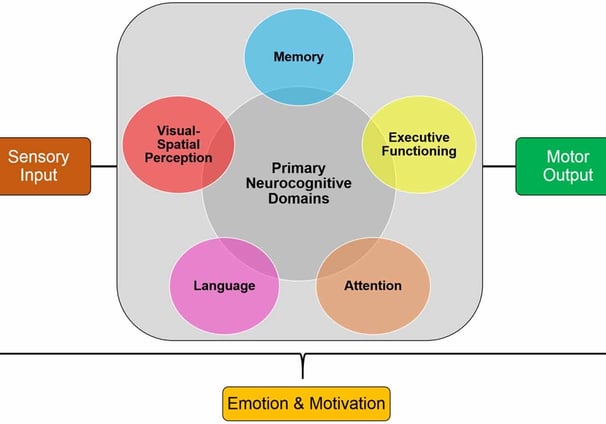
More comprehensive neuropsychological testing batteries are often used to evaluate multiple cognitive domains in depth. There is some debate among experts about which specific tests are best for diagnosing MCI. Most agree that assessing multiple cognitive domains is important, rather than relying on a single screening test.
Recent research has also focused on identifying biomarkers that may help diagnose MCI and predict progression to dementia. Brain imaging techniques like MRI and PET scans can detect structural and functional changes associated with cognitive decline. Cerebrospinal fluid tests for proteins like amyloid and tau may also provide useful diagnostic information. However, the use of these biomarker tests is still primarily in the research realm and not yet widely implemented in routine clinical practice.
Managing and Treating MCI
Receiving a diagnosis of MCI can understandably cause anxiety for patients and families. However, identifying cognitive decline at this early stage provides an important window of opportunity. With proper management, it may be possible to slow progression and maintain independence for longer.
Currently, there are no FDA-approved medications specifically for treating MCI. Some of the key approaches for managing MCI include:
Lifestyle Modifications:
Regular physical exercise (aim for 150 minutes of moderate aerobic activity per week)
Cognitive stimulation and mentally engaging activities
Social engagement
A healthy diet (Mediterranean-style diets show promise for brain health)
Adequate sleep
Stress reduction techniques like meditation
Medical Management:
Treating underlying health conditions that may contribute to cognitive decline (e.g. high blood pressure, diabetes, sleep apnea)
Reviewing and adjusting medications that may cause cognitive side effects
Managing depression, anxiety or other mental health issues
Treating sensory deficits like hearing loss
Cognitive Training:
Memory improvement strategies and techniques
Cognitive rehabilitation exercises
Computer-based brain training programs (evidence is mixed on effectiveness)
Safety Planning:
Home safety assessment and modifications if needed
Driving evaluation
Advance care planning and legal/financial preparations
While there are no approved pharmacological treatments specifically for MCI, some doctors may consider prescribing medications off-label in certain cases. Cholinesterase inhibitors like donepezil, which are used to treat Alzheimer's disease, have shown mixed results in MCI clinical trials. Most experts do not recommend routine use of these drugs for MCI due to limited evidence of benefit.
Some promising areas of research for MCI treatment include:
Ginkgo biloba extract (EGb761) - some studies show potential cognitive benefits
Traditional Chinese herbal medicines - preliminary research shows promise but more rigorous studies needed
Novel drug therapies targeting brain inflammation, vascular health, and protein aggregation
Non-invasive brain stimulation techniques
The key is to work closely with your doctor to develop a personalized management plan tailored to your specific symptoms, risk factors and health status.
Monitoring and Follow-Up
For individuals diagnosed with MCI, regular monitoring is important to track symptoms and catch any progression to dementia early. Most experts recommend follow-up cognitive evaluations every 6–12 months. However, there is no clear consensus on the optimal frequency of monitoring or which specific assessments should be used in follow-up.
Patients and families should stay alert for any changes in cognitive abilities or daily functioning between doctor visits. Keeping a symptom diary can be helpful. It's also important to maintain open communication with your health care team and report any new concerns promptly.
Living Well with MCI
While an MCI diagnosis can feel scary, it's important to remember that cognitive decline is not inevitable. Many people with MCI remain stable for years or even show improvements in cognition over time. Focusing on brain-healthy lifestyle habits, staying socially and mentally active, and working closely with your medical team can help maximize your cognitive health.
Some tips for living well with MCI include:
- Stay positive and focus on what you can do, rather than limitations
Establish routines and use memory aids like calendars, to-do lists and reminders
Break tasks into smaller steps if needed
Reduce distractions and clutter in your environment
Ask for help when you need it
Prioritize self-care, including exercise, nutrition and stress management
Stay connected with family and friends
Pursue hobbies and activities you enjoy
Consider joining a support group for people with MCI
It's also important for family members and caregivers to educate themselves about MCI and learn strategies to support their loved one. Patience, understanding and maintaining a sense of normalcy are keys.
The Importance of Early Detection
Identifying cognitive changes early provides the best opportunity for effective intervention and planning. If you have concerns about your cognitive health or that of a loved one, don't hesitate to speak with a doctor. Some key reasons why early detection of MCI is beneficial include:
Opportunity to address reversible causes: Some cases of MCI may be caused by treatable conditions like vitamin deficiencies, thyroid problems or medication side effects.
The window for lifestyle interventions: Adopting brain-healthy habits early may help slow the progression of cognitive decline.
Time for planning: Early diagnosis allows individuals to actively make decisions about future care and legal/financial planning.
Access to clinical trials: People with early-stage MCI may be eligible to participate in research studies testing new treatments.
Better management of other health conditions - MCI may complicate management of other chronic diseases, so early detection allows for proactive care coordination.
Ongoing Research and Future Directions
Mild cognitive impairment remains an active area of research, with scientists working to better understand its causes, improve diagnostic methods, and develop effective treatments. Some key areas of ongoing research include:
Identifying genetic and environmental risk factors for MCI
Developing more sensitive cognitive tests and biomarkers for early detection
Understanding the biological mechanisms underlying cognitive decline
Conclusion
Mild cognitive impairment represents an important transitional stage between normal cognitive aging and dementia. While a diagnosis of MCI can be concerning, it also provides a crucial opportunity for early intervention. By understanding the signs of MCI, seeking prompt medical evaluation when needed, and taking a proactive approach to brain health, we can work to maintain cognitive function and quality of life as we age. If you have concerns about cognitive changes in yourself or a loved one, don't hesitate to speak with a healthcare provider. With proper care and support, many people with MCI are able to maintain their independence and continue living rich, fulfilling lives. As research advances, we can look forward to better tools for early detection and more effective treatment options on the horizon.
Faqs
Can someone recover from mild cognitive impairment?
A: Mild cognitive impairment (MCI) may improve in some cases, remain stable, or progress to dementia. Recovery depends on the underlying cause, and in some cases, cognitive function can improve, especially with treatment and lifestyle changes.
Q: How do you improve mild cognitive impairment?
A: Improving mild cognitive impairment may involve engaging in mentally stimulating activities such as playing games, playing an instrument, or reading books. Social interaction, memory training, and cognitive training exercises may also help preserve brain function and slow mental decline.
Q: Does MCI always lead to dementia?
A: No, MCI does not always lead to dementia. Some people with MCI may never develop dementia, while others may see their condition progress. The outcome can vary widely depending on the individual.
Q: What is the life expectancy with mild cognitive impairment?
A: Life expectancy for individuals with mild cognitive impairment varies and is often similar to those without MCI, especially if the condition does not progress to dementia. However, if MCI progresses to dementia, life expectancy may be affected depending on the type and severity of dementia.
Q: Is mild cognitive impairment permanent?
A: MCI is not always permanent. In some cases, cognitive function may improve, particularly if the impairment is due to a treatable cause. In other cases, it may remain stable or progress to a more severe condition like dementia.
Journal Reference
Chen, X., Liang, N., Li, L., Yang, H., Wang, P., & Shi, N. (2021). Diagnosis and Treatment for Mild Cognitive Impairment: A Systematic Review of Clinical Practice Guidelines and Consensus Statements. Frontiers in Neurology, 12. https://doi.org/10.3389/fneur.2021.719849
Image credit: https://www.frontiersin.org/files/Articles/434855/fnbeh-13-00048-HTML/image_m/fnbeh-13-00048-g001.jpg
Related:
https://healthnewstrend.com/diet-and-dementia-swap-red-meat-for-nuts-to-lower-dementia-risk
Disclaimer
The information on this website is for informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health care provider with any questions you may have regarding a medical condition or treatment. Never disregard professional medical advice or delay in seeking it because of something you have read on this website
