Brain Insulin: The Secret Weapon for Weight Management, Mood & Brain Health
Struggling with weight, mood, or memory? Brain insulin might be the missing piece. Discover how this powerful hormone regulates metabolism, appetite, and cognitive function. Learn about brain insulin resistance and promising solutions to optimize your health.
DR T S DIDWAL MD
4/1/20246 min read
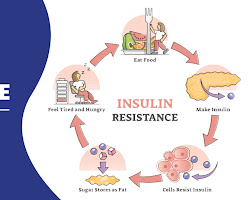
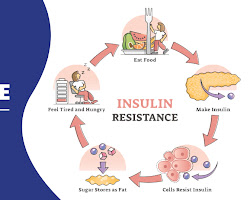
Brain insulin once thought to only regulate blood sugar, plays a surprising role as a conductor of your overall health. It influences how your body uses energy, curbs cravings, and even impacts mood and memory. According to research in Diabetologia, when the brain becomes resistant to insulin's messages, a condition called brain insulin resistance, can disrupt metabolism and potentially contribute to weight gain, diabetes, and even neurological disorders. Exciting research suggests that exercise, certain medications, and future advancements could improve brain insulin action, offering a potential key to better weight management, mental well-being, and overall health.
Key Points
Insulin's Role in the Brain
This review discusses recent findings on how insulin, a hormone known for regulating blood sugar, also acts in the human brain. It emphasizes research specifically done in humans.
How Insulin Gets into the Brain
The brain is protected by a blood-brain barrier (BBB) that restricts what enters. Insulin uses specific mechanisms to cross the BBB and reach brain cells. The effectiveness of this transport can vary depending on factors like age and obesity.
Evidence of Brain Insulin Action
Scientists use various techniques to stimulate brain insulin action and measure its effects. These techniques include monitoring brain activity after meals (natural insulin release), injecting insulin directly into the bloodstream, and administering insulin through the nose (which delivers it more directly to the brain). Brain imaging techniques like fMRI help researchers see which brain regions are activated by insulin.
Studies have shown that insulin affects several brain areas involved in functions like:
Energy metabolism: Regulating how the body uses energy.
Eating behavior: Influencing hunger and satiety (feeling full).
Reward processing: motivating us to seek pleasurable things like food.
Mood regulation: affecting emotions.
Cognitive functions: include memory and decision-making.
Brain Insulin Resistance
Just like the body can become resistant to insulin's effects on blood sugar, the brain can also become resistant. This means the brain doesn't respond as well to insulin signals. Brain insulin resistance is linked to:
Overweight and obesity
Normal aging
High levels of certain fats (NEFAs) in the blood
Genetics
Sex Differences in Brain Insulin Action
Early research suggests some sex differences in how the brain responds to insulin. For example, women's hypothalamic insulin sensitivity might change throughout the menstrual cycle.
Potential Benefits of Enhancing Brain Insulin Action
Studies using nasal insulin delivery have shown promise in improving memory, regulating eating behavior, and influencing mood in some people.
Future Directions
This research area is still developing. Scientists are looking for ways to:
Develop better methods to measure brain insulin sensitivity.
Understand the long-term consequences of brain insulin resistance.
Identify potential treatments to improve brain insulin action and potentially improve overall health and well-being.
Overall Significance
This review highlights the growing body of evidence that insulin plays a significant role in human brain function. Understanding brain insulin action could lead to novel therapies for obesity, diabetes, and even age-related cognitive decline.
For a long time, we thought insulin only worked in the periphery, regulating blood sugar by telling our cells to absorb glucose. But recent research reveals a fascinating twist: insulin also acts potently within the brain, influencing how our bodies manage energy. This blog post dives deep into the world of brain insulin action, exploring its effects on peripheral metabolism and the potential consequences of brain insulin resistance. The brain is a privileged organ, protected by a blood-brain barrier (BBB) that restricts what enters. However, insulin uses specific mechanisms to cross the BBB and reach brain cells. Interestingly, the effectiveness of this transport can vary depending on factors like age and obesity.
Brain Insulin's Many Hats
Scientists use various techniques to stimulate brain insulin action and measure its effects. These techniques involve monitoring brain activity after meals (natural insulin release), injecting insulin directly into the bloodstream, and delivering it through the nose (which delivers it more directly to the brain). Studies have shown that brain insulin plays a role in several key areas:
Energy Metabolism: It regulates how the body uses energy, influencing how efficiently we burn fuel.
Eating Behavior: It affects hunger and satiety (feeling full) by influencing appetite centers in the brain.
Reward Processing: It motivates us to seek pleasurable things like food by activating reward pathways.
Mood Regulation: It impacts emotions, potentially influencing mood disorders.
Cognitive Functions: It might play a role in memory, learning, and decision-making.
Brain Insulin Resistance: When the Signal Goes Unheard
Just like the body can become resistant to insulin's effects on blood sugar, the brain can also become resistant. This means the brain doesn't respond as well to insulin's signals. Brain insulin resistance is linked to:
Overweight and obesity
Normal aging
High levels of certain fats (NEFAs) in the blood
Genetics
Sex Differences: Does Gender Matter?
Early research suggests some sex differences in how the brain responds to insulin. For example, women's hypothalamic insulin sensitivity might change throughout the menstrual cycle.
Potential Benefits of Boosting Brain Insulin Action
Studies using nasal insulin delivery show promise in improving memory, regulating eating behavior, and influencing mood in some people. These findings suggest that enhancing brain insulin action could be a potential therapeutic avenue.
The Big Picture: Brain Insulin and Peripheral Metabolism
While the research on brain insulin's effects on the brain itself is fascinating, its influence extends beyond the skull. Here's how brain insulin action impacts how our bodies handle energy:
Suppressing Glucose Production: Brain insulin helps regulate how much glucose the liver produces.
Enhancing Liver Function: It improves liver energy metabolism and reduces liver fat content.
Promoting Glucose Uptake: It stimulates peripheral glucose uptake, particularly in muscle and adipose tissue.
Boosting Insulin Secretion: It acutely enhances insulin secretion from the pancreas, further aiding blood sugar control.
Brain Insulin Resistance and Its Potential Impact
Importantly, these positive effects of brain insulin action on peripheral metabolism seem to be diminished or absent in people who are overweight, obese, or have brain insulin resistance or type 2 diabetes. This suggests a potential link between impaired brain insulin action and metabolic disorders.
Brain Insulin Resistance: A Potential Culprit?
Long-term consequences of brain insulin resistance are still being explored, but some studies suggest potential connections to:
Visceral Obesity: This unhealthy fat distribution around the organs might be linked to brain insulin resistance.
Metabolic Diseases: Brain insulin resistance could contribute to the development of type 2 diabetes and other metabolic problems.
Neurological and Psychiatric Disorders: Potential links have been found between brain insulin resistance and conditions like Alzheimer's disease, Parkinson's disease, and depression.
Treatment Options: Can We Fix Brain Insulin Resistance?
Given the potential consequences of brain insulin resistance, treatments are being explored. While human studies are scarce, some initial research shows promise:
Exercise: Regular physical activity, even without significant weight loss, can improve brain insulin responsiveness.
Medications: SGLT2 inhibitor drugs, used for type 2 diabetes, might improve brain insulin sensitivity in some cases.
The Road Ahead: Unlocking the Mysteries of Brain Insulin
Research on brain insulin action is a rapidly evolving field with many exciting possibilities. Here are some key areas for future exploration:
Understanding Communication: Deciphering how the brain talks to peripheral organs like the liver and muscles in response to insulin.
Brain Insulin Transport: Unraveling the mechanisms that control how insulin gets into the brain.
Development of Biomarkers: Identifying reliable and accessible tools to diagnose brain insulin resistance.
Untangling the Intricate Communication Network:
The communication between the brain and peripheral organs like the liver, muscles, and pancreas is a fascinating dance. Understanding how brain insulin action translates into signals for these organs is crucial. Researchers are looking at the role of the autonomic nervous system and potential circulating factors in this intricate conversation.
Is insulin the only player?
Insulin might be the lead singer in the brain's metabolic orchestra, but are there other players involved? Exploring how other hormones and signaling molecules interact with insulin within the brain could provide a more complete picture. Additionally, investigating how factors like leptin, which informs the brain about energy availability, influence this delicate balance is essential.
Brain Insulin Resistance and Disease: Cause or Consequence?
Does impaired brain insulin action contribute to the development of high-risk phenotypes in prediabetes and diabetes, neurological disorders, and psychiatric conditions, or is it a consequence of these conditions? Delving deeper into this question will help us understand the root cause of these issues and develop more effective preventive and intervention strategies.
The Search for Biomarkers: Simplifying Diagnosis
Currently, diagnosing brain insulin resistance often involves expensive and time-consuming techniques like fMRI with nasal insulin administration. Developing accessible, non-invasive tools like blood tests, digital measures, or combinations thereof would be a game-changer. This would allow for easier diagnosis, accurate risk stratification, and monitoring of treatment response.
Optimizing Treatments for a Broader Impact
Refining and optimizing treatment methods for brain insulin resistance could open new avenues for prevention and therapy, not just for obesity and metabolic disorders but also for related neurological and psychiatric conditions. Exploring the potential of existing medications, lifestyle interventions, and even novel approaches specifically targeting brain insulin action holds immense promise.
Conclusion: A Symphony of Hope
The exploration of brain insulin action is transforming our understanding of metabolism and its complex relationship with the brain. This exciting field of research holds the potential to revolutionize how we approach not only metabolic disorders but also neurological and psychiatric conditions. By unravelling the intricate melodies within the brain insulin symphony, we can unlock a world of possibilities for improving human health and well-being.
Journal Reference
Heni, M. The insulin resistant brain: impact on whole-body metabolism and body fat distribution. Diabetologia (2024). https://doi.org/10.1007/s00125-024-06104-9
Disclaimer The information on this website is for informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health care provider with any questions you may have regarding a medical condition or treatment. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
