Type 2 Diabetes & Fatty Liver Disease: SGLT2 Inhibitors Show Promise as Top Treatment
Struggling with both type 2 diabetes and fatty liver disease? New research suggests SGLT2 inhibitors might be the best option for managing both conditions. Learn more about the benefits and the need for further studies.
DR T S DIDWAL MD
3/31/20245 min read
A new study in JAMA Internal Medicine suggests SGLT2 inhibitors might be the best oral medication for patients struggling with both type 2 diabetes (T2D) and nonalcoholic fatty liver disease (NAFLD). The research, involving over 80,000 patients, found that SGLT2 inhibitors were linked to a nearly 99% higher chance of NAFLD improvement compared to other medications. Additionally, they were associated with a 63% reduction in serious liver complications. While the exact reasons for this benefit are unclear, SGLT2 inhibitors may influence fat metabolism and weight loss, factors crucial for NAFLD management. Though further research is needed to confirm these findings, this study highlights the potential of SGLT2 inhibitors as a game-changer for managing NAFLD in T2D patients.
Key Points
This study investigated which class of oral antidiabetic drugs (OADs) is most beneficial for patients with both type 2 diabetes (T2D) and nonalcoholic fatty liver disease (NAFLD).
Background:
Several OADs exist, and their effects on NAFLD vary.
Limited clinical data exists on which class is best for patients with both conditions.
Objective:
To identify the OAD associated with the most favourable outcomes in NAFLD and T2D patients.
Study Design:
a retrospective, non-randomized cohort study using a large Korean national database.
Analyzed data from 80,178 patients diagnosed with both T2D and NAFLD.
The follow-up period spanned 219,941 person-years.
Treatments Considered:
Patients were categorized based on the OAD they received along with metformin (used in 80% of cases for at least 90 days). The OADs were:
Sodium-glucose cotransporter 2 (SGLT2) inhibitors
Thiazolidinediones
Dipeptidyl peptidase-4 (DPP-4) inhibitors
Sulfonylureas (used as the comparison group)
Results:
Patients were followed for an average of 58.5 years.
A total of 4,102 patients experienced NAFLD regression.
Compared to sulfonylureas, all other OAD groups showed a higher likelihood of NAFLD regression:
SGLT2 inhibitors: 99% higher chance (ASHR 1.99, 95% CI 1.75-2.27)
Thiazolidinediones: 70% higher chance (ASHR 1.70, 95% CI 1.41-2.05)
DPP-4 inhibitors: 45% higher chance (ASHR 1.45, 95% CI 1.31–1.59)
SGLT2 inhibitors had a significantly higher chance of NAFLD regression compared to both thiazolidinediones (40% higher, ASHR 1.40) and DPP-4 inhibitors (45% higher, ASHR 1.45).
Only SGLT2 inhibitors showed a significantly lower incidence of adverse liver-related outcomes compared to sulfonylureas (63% reduction, ASHR 0.37). Neither thiazolidinediones nor DPP-4 inhibitors had this effect.
Conclusions:
This study suggests SGLT2 inhibitors may be the preferred OAD for patients with T2D and NAFLD due to their potential benefits for NAFLD regression and reduced risk of liver complications.
This observational study encourages further research to confirm these findings and potentially change prescribing practices for this patient population.
For patients struggling with both type 2 diabetes (T2D) and nonalcoholic fatty liver disease (NAFLD), navigating treatment options can be challenging. Several oral antidiabetic drugs (OADs) exist, but their impact on NAFLD varies. A recent study published in Diabetic Research and Clinical Practice sheds light on this by investigating which OAD class might be most beneficial. This blog post delves into the study's findings and explores the potential of SGLT2 inhibitors for managing this complex co-morbidity.
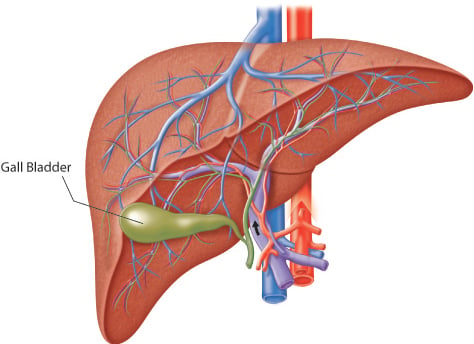
The Burden of NAFLD and T2D:
NAFLD, characterized by excess fat accumulation in the liver, is a rapidly growing health concern. It often co-occurs with T2D, a chronic condition marked by high blood sugar levels. This co-existence poses a significant risk for both diseases to progress, potentially leading to severe complications like liver cirrhosis and cardiovascular disease.
Unveiling the Potential of SGLT2 Inhibitors:
The Korean study, involving over 80,000 patients with T2D and NAFLD, compared the effectiveness of four OAD classes: SGLT2 inhibitors, thiazolidinediones, DPP-4 inhibitors, and sulfonylureas (the control group). All OADs were used in combination with metformin.
The researchers focused on two key outcomes: NAFLD regression, assessed by the fatty liver index, and a composite of adverse liver-related events (hospitalization, mortality, transplant, or hepatocellular carcinoma).
The findings were promising for SGLT2 inhibitors:
Compared to sulfonylureas, SGLT2 inhibitors were associated with a nearly 99% higher chance of NAFLD regression (adjusted subdistribution hazard ratio [ASHR] 1.99, 95% CI 1.75-2.27)
They also showed a significantly lower incidence of adverse liver-related outcomes (63% reduction, ASHR 0.37) compared to sulfonylureas
Interestingly, SGLT2 inhibitors demonstrated better results for NAFLD regression than both thiazolidinediones (40% higher, ASHR 1.40) and DPP-4 inhibitors (45% higher, ASHR 1.45)
Understanding the Mechanism:
While the exact mechanism of SGLT2 inhibitors in NAFLD remains under investigation, several factors may contribute to their effectiveness:
SGLT2 inhibitors work by promoting the excretion of excess glucose through the urine, potentially leading to weight loss and improved insulin sensitivity, both of which are beneficial for NAFLD management
They may also influence key metabolic pathways in the liver, reducing fat production and promoting fat breakdown
A Call for Further Research:
This study, though robust, has limitations inherent to its observational design. Randomized controlled trials are needed to definitively establish a cause-and-effect relationship between SGLT2 inhibitors and improved NAFLD outcomes. Additionally, the research was conducted on a Korean population, and generalizability to other ethnicities requires further exploration.
Looking Ahead: A Potential Shift in Prescribing Practices?
Despite these limitations, the study offers exciting insights. The observed benefits of SGLT2 inhibitors for NAFLD regression and reduced liver complications warrant further investigation. If future studies confirm these findings, it could lead to a shift in prescribing practices for patients with T2D and NAFLD.
This potential shift is further supported by the established benefits of SGLT2 inhibitors in managing T2D itself. These drugs have demonstrated effectiveness in lowering blood sugar levels, reducing cardiovascular risks, and protecting kidney function
Empowering Patients and Providers:
While this study highlights the promise of SGLT2 inhibitors, it's crucial to remember that treatment decisions should be individualized and made in consultation with a healthcare professional. Factors like medication side effects, individual health conditions, and overall treatment goals must be considered.
Future Directions:
Research efforts are ongoing to explore the multifaceted effects of SGLT2 inhibitors on NAFLD. Studies are investigating the optimal duration of treatment, potential combinations of therapies with other medications, and the long-term impact on liver health.
Conclusion:
The growing body of evidence, including this recent Korean study, suggests that SGLT2 inhibitors may hold significant promise for managing NAFLD in patients with T2D. Their potential to improve NAFLD regression, alongside their established benefits for T2D management, warrants further research and consideration in clinical practice. As knowledge in this area evolves, healthcare providers will be better equipped to offer personalized treatment plans, empowering patients with T2D and NAFLD to achieve optimal health outcomes.
Journal Reference
Jang, H., Kim, Y., Lee, D. H., Joo, S. K., Koo, B. K., Lim, S., Lee, W., & Kim, W. (2024, February 12). Outcomes of Various Classes of Oral Antidiabetic Drugs on Nonalcoholic Fatty Liver Disease. JAMA Internal Medicine. https://doi.org/10.1001/jamainternmed.2023.8029
Related
Medical Disclaimer
The information on this website is for informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition or treatment. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
