Is Obesity Affecting Your Fertility? Link Between Weight and Women's Reproductive Health
Discover the complex relationship between obesity and female fertility. Learn how excess weight can impact reproductive health and explore effective strategies for improving fertility outcomes.
DR T S DIDWAL MD
10/18/20247 min read
The intricate relationship between obesity and female fertility is a complex interplay of hormonal imbalances, metabolic disruptions, and reproductive system changes. According to a review in Frontiers in endocrinology ,obesity can affect fertility through various mechanisms, including hormonal disruption, metabolic changes, and reproductive system effects. These alterations can lead to irregular menstrual cycles, difficulties with ovulation, and increased risk of pregnancy complications. While obesity can pose significant challenges to fertility, management strategies such as lifestyle modifications and medical interventions can help address these issues. Early intervention, comprehensive treatment approaches, and consistent healthcare support are crucial for achieving positive outcomes in managing both obesity and fertility concerns.
Keypoints
Obesity is a significant factor affecting female fertility. Approximately one-third of women in their reproductive years are affected by obesity, making this a critical issue in reproductive medicine.
Obesity impacts fertility through multiple mechanisms. These include hormonal disruption, metabolic changes, and reproductive system effects.
Hormonal imbalances play a key role. Obesity can alter levels of key reproductive hormones, disrupt menstrual cycles, and impair ovulation.
Metabolic changes can also affect fertility. Insulin resistance, altered glucose metabolism, and changes in fat tissue function can impact reproductive health.
Reproductive system effects include compromised oocyte quality, altered endometrial receptivity, and increased risk of miscarriage.
Management strategies for obesity-related fertility issues include lifestyle modifications and medical interventions. These can help address weight management, hormonal imbalances, and other factors affecting fertility.
Early intervention and consistent healthcare support are crucial. Addressing obesity-related fertility issues early on can improve outcomes and increase the chances of successful conception.
The Complex Relationship Between Obesity and Female Fertility: A Comprehensive Overview
In recent years, the connection between obesity and female fertility has become an increasingly important area of study in reproductive medicine. With approximately one-third of women in their reproductive years affected by obesity, understanding this relationship is crucial for both healthcare providers and patients. This comprehensive overview explores how obesity impacts female fertility and what can be done about it. Obesity affects female fertility through multiple complex mechanisms, creating a perfect storm of hormonal imbalances, metabolic disruptions, and reproductive system changes. These alterations can lead to various fertility challenges, including irregular menstrual cycles, difficulties with ovulation, and increased risk of pregnancy complications.
Key Impact Areas
Hormonal Disruption
Altered levels of key reproductive hormones
Disrupted menstrual cycles
Impaired ovulation processes
Changes in sex hormone-binding globulin (SHBG) levels
Metabolic Changes
Insulin resistance
Altered glucose metabolism
Changes in fat tissue function
Disrupted energy balance
Reproductive System Effects
Compromised oocyte quality
Altered endometrial receptivity
Increased risk of miscarriage
Reduced success rates in assisted reproduction
The Role of Hormones and Adipokines
Leptin: The Satiety Hormone
Leptin plays a crucial role in both energy balance and reproductive function. In obesity, despite high leptin levels, individuals often develop leptin resistance. This condition affects:
The onset and regulation of puberty
Normal reproductive cycle functioning
Oocyte development and quality
Embryo-endometrial interactions
Adiponectin: The Insulin Sensitizer
Adiponectin levels typically decrease in obesity, leading to:
Reduced insulin sensitivity
Altered ovarian function
Compromised follicular development
Changed reproductive hormone production
Ghrelin: The Hunger Hormone
Obesity affects ghrelin levels, which impacts:
Reproductive axis function
Ovarian hormone production
Fertility treatment outcomes
Puberty timing and progression
The Inflammatory Connection
Obesity creates a state of chronic low-grade inflammation that can significantly impact fertility. Key inflammatory markers include:
TNF-α (Tumor Necrosis Factor-alpha)
Elevated in obesity
Affects insulin sensitivity
Impacts ovarian function
Influences embryo development
Interleukin-6 (IL-6)
Increased in obese individuals
Affects reproductive hormone production
Influences endometrial receptivity
Impacts pregnancy outcomes
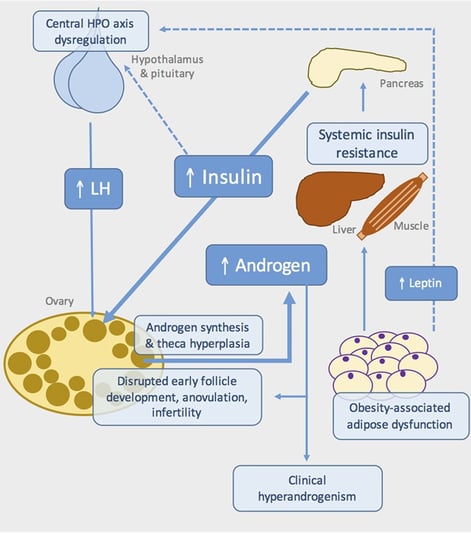
Obesity and Polycystic Ovary Syndrome (PCOS)
Obesity and Polycystic Ovary Syndrome (PCOS) have a complex, bidirectional relationship where each condition can exacerbate the other. This note explores their interconnection and clinical implications.
Pathophysiological Connection
Insulin Resistance
Common feature in both conditions
Creates a cyclical relationship where obesity worsens insulin resistance
Contributes to increased androgen production in PCOS
Hormonal Imbalance
Elevated androgens in PCOS promote central adiposity
Excess adipose tissue increases estrogen production
Disrupted hormonal balance affects metabolic function
Clinical Impact
1. Weight Management Challenges
PCOS makes weight loss more difficult
Insulin resistance promotes fat storage
Metabolic rate may be affected
2. Reproductive Health
Both conditions contribute to fertility issues
Irregular menstrual cycles
Increased risk of pregnancy complications
The Gut Microbiome Factor
Recent research has highlighted the importance of gut microbiota in both obesity and fertility. Obesity-related dysbiosis can:
Alter hormone metabolism
Affect inflammatory responses
Impact reproductive function
Influence pregnancy outcomes
Impact on Assisted Reproduction
Obesity can significantly affect the success rates of assisted reproductive technologies:
IVF Outcomes
Reduced pregnancy rates
Higher medication requirements
Increased cycle cancellation rates
Higher miscarriage risks
Specific Challenges
Compromised oocyte quality
Altered endometrial receptivity
Reduced implantation rates
Increased pregnancy complications
Management Strategies
Lifestyle Modifications
Dietary Changes
Reduced caloric intake
Balanced macronutrient composition
Increased fiber intake
Limited processed foods
Physical Activity
Regular exercise routines
Combination of aerobic and strength training
Consistent activity schedule
Gradual intensity increase
Medical Interventions
Pharmacotherapy
Weight management medications
Fertility medications
Insulin sensitizers
Hormone treatments
Bariatric Surgery
For severe cases, bariatric surgery might be considered, which can:
Significantly reduce weight
Improve hormone balance
Restore regular menstruation
Enhance fertility outcomes
Prevention and Early Intervention
The best approach to managing obesity-related fertility issues is prevention:
Early Warning Signs
Irregular menstrual cycles
Unexplained weight gain
Changes in energy levels
Difficulty conceiving
Preventive Measures
Regular health monitoring
Maintaining healthy weight
Balanced nutrition
Regular physical activity
The Role of Healthcare Providers
Healthcare providers play a crucial role in:
Early identification of risk factors
Regular monitoring of weight and metabolic health
Providing appropriate interventions
Offering support and guidance
The Real-Life Impact of Obesity on Fertility: Sarah's Journey
Sarah, a 32-year-old woman from Denver, had always dreamed of starting a family. But after trying to conceive for over two years without success, she began to worry. Despite tracking her ovulation and leading what she thought was a healthy lifestyle, Sarah was struggling. She felt disheartened and unsure of what was going wrong.
After consulting with her doctor, Sarah learned that her weight might be contributing to her fertility challenges. She had never considered how her body weight might be affecting her reproductive health. Her doctor explained that obesity could lead to hormonal imbalances, making it harder for her to ovulate regularly. In fact, Sarah’s weight had been silently influencing her menstrual cycle for years.
Determined to take action, Sarah embarked on a personalized weight management plan that combined a healthier diet with regular exercise. She worked closely with her healthcare team, who monitored her progress and offered ongoing support. Over the next year, Sarah not only lost weight but also saw improvements in her ovulation cycles. After months of effort, Sarah finally received the news she had been waiting for—she was pregnant.
Conclusion
The relationship between obesity and female fertility is complex and multifaceted. Understanding these connections is crucial for both healthcare providers and patients. While obesity can significantly impact fertility, various management strategies are available. The key lies in early intervention, comprehensive treatment approaches, and consistent monitoring.
For women struggling with both obesity and fertility issues, hope lies in the many available treatment options and management strategies. Success often comes from a combination of approaches, including lifestyle modifications, medical interventions when necessary, and consistent healthcare support.
Remember that each person's journey is unique, and what works for one may not work for another. Working closely with healthcare providers to develop personalized treatment plans is crucial for achieving the best possible outcomes in managing both obesity and fertility concerns.
FAQs
1. What is the connection between obesity and female fertility?
Obesity can significantly impact female fertility through various mechanisms, including hormonal disruption, metabolic changes, and reproductive system effects. These changes can lead to irregular menstrual cycles, difficulties with ovulation, and increased risk of pregnancy complications.
2. How does obesity affect hormones and fertility?
Obesity can disrupt hormonal balance, affecting key reproductive hormones like estrogen and progesterone. This can lead to irregular menstrual cycles, impaired ovulation, and altered endometrial receptivity. Additionally, obesity can influence the production of adipokines, hormones secreted by fat tissue, which can further impact fertility.
3. Can obesity increase the risk of miscarriage?
Yes, obesity can increase the risk of miscarriage. This is due to factors such as compromised oocyte quality, altered endometrial receptivity, and increased inflammation associated with obesity.
4. What are the treatment options for obesity-related fertility issues?
Treatment options for obesity-related fertility issues often involve a combination of lifestyle modifications and medical interventions. Lifestyle modifications include dietary changes, regular physical activity, and weight management. Medical interventions may include fertility medications, insulin sensitizers, or in severe cases, bariatric surgery.
5. Can fertility treatments be successful for women with obesity?
While obesity can present challenges for fertility treatments, success is still possible. However, it may require more intensive treatment plans and potentially higher medication dosages.
6. Is it possible to prevent obesity-related fertility issues?
Yes, preventing obesity-related fertility issues is possible through healthy lifestyle choices. Maintaining a healthy weight, eating a balanced diet, and engaging in regular physical activity can significantly reduce the risk of fertility problems associated with obesity.
7. Should women with obesity seek early medical attention?
Yes, women with obesity should seek early medical attention to discuss their fertility concerns. Early intervention can help identify potential issues and develop appropriate treatment plans to improve fertility outcomes.
8. Are there any fertility-related risks associated with losing weight too quickly?
Rapid weight loss can be detrimental to fertility. It can disrupt hormonal balance and lead to irregular menstrual cycles. Gradual and sustainable weight loss is generally recommended for optimal fertility outcomes.
9. Can fertility improve after weight loss?
Yes, fertility can improve after weight loss. By addressing obesity-related factors, such as hormonal imbalances and metabolic changes, weight loss can positively impact reproductive health.
10. Is there a specific age at which obesity becomes a greater concern for fertility?
While obesity can affect fertility at any age, it may become a more significant concern as women approach their late 30s and early 40s. This is due to the natural decline in fertility that occurs with age.
Related Article
PCOS: How to Overcome Fertility, Health, and Cardiometabolic Risks?
Journal references
Baraskar, K., Thakur, P., Shrivastava, R., & Shrivastava, V. K. (2021). Female obesity: Association with endocrine disruption and reproductive dysfunction. Obesity Medicine, 28, 100375. https://doi.org/10.1016/j.obmed.2021.100375
Marinelli, S., Napoletano, G., Straccamore, M., & Basile, G. (2022). Female obesity and infertility: outcomes and regulatory guidance. Acta bio-medica : Atenei Parmensis, 93(4), e2022278. https://doi.org/10.23750/abm.v93i4.13466
Uddandrao, V. V., Brahma Naidu, P., Chandrasekaran, P., & Saravanan, G. (2024). Pathophysiology of obesity-related infertility and its prevention and treatment by potential phytotherapeutics. International Journal of Obesity, 48(2), 147-165. https://doi.org/10.1038/s41366-023-01411-4
Zheng, L., Yang, L., Guo, Z., Yao, N., Zhang, S., & Pu, P. (2024). Obesity and its impact on female reproductive health: unraveling the connections. Frontiers in endocrinology, 14, 1326546. https://doi.org/10.3389/fendo.2023.1326546
Image credit: https://www.frontiersin.org/files/Articles/202961/fendo-07-00053-HTML/image_m/fendo-07-00053-g001.jpg
Disclaimer
The information on this website is for informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health care provider with any questions you may have regarding a medical condition or treatment. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
