PCOS: How to Overcome Fertility, Health, and Cardiometabolic Risks?
Discover the hidden health challenges of polycystic ovarian syndrome (PCOS), including its impact on fertility, cardiovascular health, and metabolic function. Learn about effective strategies to manage PCOS and improve overall well-being.
DR ANITA JAMWAL MS
10/12/20248 min read
Polycystic Ovarian Syndrome (PCOS) is a complex hormonal disorder affecting millions of women. While often associated with fertility issues, PCOS also has significant implications for overall health, particularly cardiovascular risk. Research published in Cureus reveals that PCOS can lead to hypertension, insulin resistance, and other metabolic disturbances. Effective management requires a holistic approach, combining lifestyle modifications, medication, and regular monitoring. Understanding the multifaceted nature of PCOS is crucial for women to take proactive steps towards maintaining their well-being.
Key points
PCOS: A multifaceted disorder—PCOS is not just a reproductive issue but also has significant implications for metabolic and cardiovascular health.
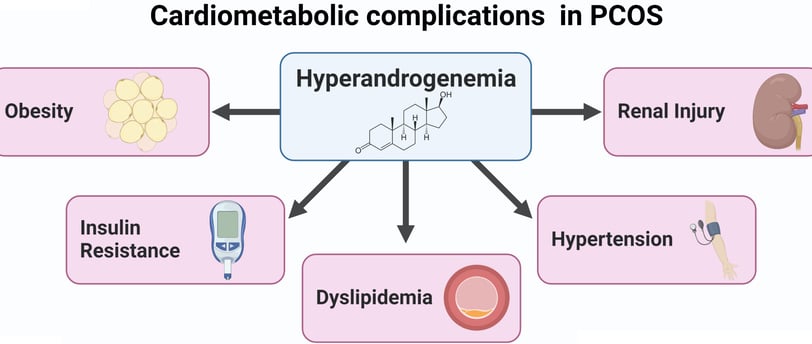
Cardiometabolic risks in PCOS: PCOS is associated with hypertension, insulin resistance, dyslipidemia, and obesity, all of which increase cardiovascular risk.
Hyperandrogenism in PCOS excessive male hormones (hyperandrogenism) is a key feature of PCOS and contributes to various symptoms and health risks.
PCOS phenotypes: PCOS presents with different phenotypes, each with unique characteristics, highlighting the diversity of the disorder.
Lifestyle modifications for PCOS - Weight loss, a healthy diet, and regular exercise can significantly improve PCOS symptoms and reduce associated health risks.
Pharmacological interventions for PCOS medications like metformin, GLP-1 receptor agonists, COCPs, and spironolactone can be effective in managing PCOS symptoms and addressing metabolic imbalances.
Regular monitoring for PCOS: Women with PCOS should undergo regular monitoring for blood pressure, metabolic parameters, and other health indicators.
Polycystic Ovarian Syndrome: More Than Just a Reproductive Issue
Polycystic Ovarian Syndrome (PCOS) is a complex endocrine disorder that affects millions of women worldwide. While it's primarily known for its impact on fertility and menstrual cycles, recent research has shed light on its far-reaching effects on overall health, particularly cardiovascular health. In this blog post, we'll dive deep into the world of PCOS, exploring its connection to hypertension and other cardiometabolic implications.
Understanding PCOS: More Than Meets the Eye
PCOS is the most common endocrine disorder in women of reproductive age, affecting approximately 6-10% of women in the United States alone. That's a staggering 7 million women! But what exactly is PCOS?
At its core, PCOS is characterized by three main features:
Hyperandrogenism (excess male hormones)
Ovulatory dysfunction
Polycystic ovarian morphology (PCOM)
However, not all women with PCOS will exhibit all three characteristics. In fact, the Rotterdam criteria, which are widely used for diagnosis, only require two out of these three features to be present.
The Four Faces of PCOS
Interestingly, researchers have identified four distinct phenotypes of PCOS:
Phenotype A: The "Classic" PCOS—hyperandrogenism, ovulatory dysfunction, and PCOM
Phenotype B: Hyperandrogenism and ovulatory dysfunction
Phenotype C: "OvulatoryPCOS"—Hyperandrogenism
Phenotype D: "Non-hyperandrogenic" PCOS"—ovulatory dysfunction and PCOM
This diversity in presentation highlights the complexity of PCOS and the need for personalized approaches to diagnosis and treatment.
The Hormonal Havoc: Hyperandrogenism in PCOS
One of the hallmarks of PCOS is hyperandrogenism—an excess of male hormones like testosterone. But why does this happen?
Two main theories attempt to explain this phenomenon:
The "Altered Gonadotropin Secretion Theory": This suggests that an increased frequency of gonadotropin-releasing hormone (GnRH) pulses leads to excessive luteinizing hormone (LH) and slightly elevated follicle-stimulating hormone (FSH) levels. The high LH stimulates androgen production from ovarian theca cells.
The "Functional Ovarian or Adrenal Hyperandrogenism Theory" This proposes that hyperandrogenism originates from dysregulated steroidogenesis in the ovaries or adrenal glands.
Regardless of the exact mechanism, the results are clear: up to 80% of women with PCOS show biochemical evidence of hyperandrogenism, leading to symptoms like hirsutism, acne, and male-pattern hair loss.
PCOS and Hypertension: An Unexpected Connection
While PCOS is primarily known for its reproductive effects, recent research has uncovered a concerning link between PCOS and hypertension. In fact, hypertension is 24% more prevalent in PCOS patients compared to healthy females. But how are these two conditions connected?
The Renin-Angiotensin System (RAS): A Key Player
The RAS plays a crucial role in regulating blood pressure, and interestingly, all components of this system have been identified in the human ovary. Women with PCOS show elevated levels of plasma prorenin and renin, which positively correlate with serum androgen levels.
One theory suggests that androgens may directly influence the RAS in the proximal renal tubule, leading to increased sodium reabsorption and, consequently, higher blood pressure. Another hypothesis proposes that the hyperandrogenic state in PCOS contributes to endothelial dysfunction, resulting in elevated blood pressure.
The Endothelin Connection
Endothelins, particularly endothelin-1 (ET-1), have also been implicated in the PCOS-hypertension link. Women with PCOS, both obese and non-obese, show higher levels of circulating ET-1 compared to controls. ET-1 is a potent vasoconstrictor and has been associated with various vascular diseases, including hypertension.
Metabolic Imbalances: The Perfect Storm
PCOS is often accompanied by a host of metabolic disturbances that can further contribute to hypertension risk:
Insulin Resistance: Present in 75% of lean women and 95% of obese women with PCOS, insulin resistance can lead to compensatory hyperinsulinemia. This condition affects various metabolic processes and may contribute to hypertension through multiple pathways, including stimulation of the sympathetic nervous system and interference with endothelium-dependent vasodilation.
Obesity and Visceral Fat Accumulation: Women with PCOS tend to accumulate visceral abdominal fat, leading to chronic low-grade inflammation. This inflammatory state, characterized by elevated markers like C-reactive protein (CRP) and interleukin-6 (IL-6), can increase metabolic risk regardless of BMI.
Dyslipidemia: The most prevalent metabolic abnormality in PCOS, dyslipidemia contributes to endothelial dysfunction and higher systolic and diastolic blood pressure.
Metabolic Syndrome: The prevalence of metabolic syndrome in women with PCOS is approximately twice as high as in age and BMI-matched control populations. This syndrome, which includes elevated blood pressure as one of its defining features, further increases cardiovascular risk in PCOS patients.
Beyond Hypertension: Other Cardiovascular Concerns in PCOS
While hypertension is a significant concern, it's not the only cardiovascular issue associated with PCOS. Recent studies have uncovered other potential cardiac complications:
Left Ventricular Hypertrophy (LVH): Normotensive women with PCOS show a higher prevalence of LVH without diastolic dysfunction compared to obese women without the syndrome. This suggests that the hearts of women with PCOS undergo compensatory changes in left ventricular structure, which could be an early indicator of future diastolic dysfunction risk.
Subclinical Atherosclerosis: Women with PCOS often show signs of endothelial dysfunction, an early marker of subclinical atherosclerosis. This condition, combined with the typical dyslipidemia seen in PCOS, significantly increases the risk of cardiovascular disease.
Managing PCOS: A Holistic Approach
Given the complex nature of PCOS and its wide-ranging effects on health, management strategies need to be comprehensive and tailored to each individual. Here are some key approaches:
1. Lifestyle Modifications:
Weight Loss: Even a modest 5% reduction in initial weight can help restore regular menstruation and improve metabolic parameters.
Diet: The DASH (Dietary Approaches to Stop Hypertension) eating pattern has shown beneficial effects on weight, BMI, lipid profile, and insulin sensitivity in women with PCOS.
Exercise: Regular physical activity can improve insulin sensitivity, help with weight management, and reduce cardiovascular risk.
2. Pharmacological Interventions:
Metformin: This insulin-sensitizing drug has shown efficacy in improving insulin sensitivity, reducing dyslipidemia, and aiding in weight loss, especially in obese women with PCOS.
GLP-1 Receptor Agonists: Emerging as a new therapeutic option, drugs like liraglutide have shown promise in reducing BMI and visceral adipose tissue in women with PCOS and obesity.
Combined Oral Contraceptive Pills (COCP): These can effectively reduce free androgens and improve the levels of sex hormone-binding globulins (SHBG), which bind to androgens and reduce their bioavailability.
Spironolactone: Originally used as a potassium-sparing diuretic for hypertension, this drug has shown benefits in reducing hirsutism in women with PCOS. Its blood pressure-lowering effect can be particularly beneficial for PCOS patients with hypertension.
3. Regular Monitoring:
Blood Pressure: The 2023 international PCOS guideline update recommends measuring blood pressure at the time of PCOS diagnosis and annually thereafter.
Metabolic Screening: Given the high prevalence of metabolic disturbances in PCOS, regular screening for insulin resistance, dyslipidemia, and other metabolic parameters is crucial.
The Future of PCOS Management
As our understanding of PCOS continues to evolve, so too do the approaches to its management. Some exciting areas of future research include:
Targeted Screening Tools: Developing algorithms or tools to facilitate targeted screening for women with PCOS who are at high metabolic risk.
Metabolic Modulation in Young Women: Exploring the potential of early metabolic intervention in young women with PCOS, especially before pregnancy, to prevent the intergenerational transmission of PCOS and its associated metabolic disorders.
Personalized Medicine: Given the diverse phenotypes of PCOS, there's a growing interest in developing more personalized treatment approaches based on individual risk profiles and specific manifestations of the syndrome.
Conclusion: PCOS: A Multifaceted Challenge
Polycystic Ovarian Syndrome is far more than just a reproductive disorder. Its intricate connections with metabolic health, particularly its association with hypertension and other cardiovascular risk factors, underscore the need for a comprehensive approach to its management.
As we continue to unravel the complex web of hormonal and metabolic disturbances in PCOS, it becomes increasingly clear that early diagnosis, regular monitoring, and holistic management strategies are crucial. By addressing not just the reproductive aspects but also the metabolic and cardiovascular implications of PCOS, we can significantly improve the long-term health outcomes and quality of life for millions of women worldwide.
For women living with PCOS, this evolving understanding brings hope. It emphasizes the importance of working closely with healthcare providers to develop personalized management plans that address all aspects of the syndrome. From lifestyle modifications to targeted pharmacological interventions, there are more tools than ever to manage PCOS effectively.
As research continues to advance, we can look forward to even more refined and effective strategies for managing PCOS and its associated health risks. The future holds promise for better screening tools, more targeted interventions, and potentially even preventive strategies that could break the cycle of PCOS transmission across generations.
In the meantime, awareness is key. Understanding the far-reaching effects of PCOS beyond reproductive health can empower women to take proactive steps in managing their overall health. Regular check-ups, maintaining a healthy lifestyle, and staying informed about the latest developments in PCOS management are all crucial steps in navigating this complex condition.
PCOS may be a challenging syndrome, but with the right knowledge, support, and management strategies, women with PCOS can lead healthy, fulfilling lives. As we continue to shine a light on this common yet often misunderstood condition, we move closer to a future where PCOS is not just managed, but potentially prevented or even cured.
FAQs about Polycystic Ovarian Syndrome (PCOS)
What is PCOS? PCOS is a hormonal disorder affecting women of reproductive age. It's characterized by excess male hormones, irregular periods, and polycystic ovaries.
What are the symptoms of PCOS? Symptoms can include irregular periods, excess hair growth, acne, weight gain, infertility, and mood disorders.
How is PCOS diagnosed? Diagnosis typically involves a physical exam, blood tests to check hormone levels, and ultrasound of the ovaries.
Can PCOS cause infertility? Yes, PCOS is a common cause of infertility in women.
Can women with PCOS get pregnant? With proper treatment, many women with PCOS can get pregnant.
What are treatment options for PCOS-related infertility? Treatment options may include medication, surgery, or assisted reproductive technologies.
Is PCOS linked to other health problems? PCOS is associated with increased risk of type 2 diabetes, heart disease, stroke, and sleep apnea.
Can PCOS affect mental health? Yes, PCOS can contribute to depression, anxiety, and other mental health issues.
How can I reduce my risk of health complications associated with PCOS? Maintaining a healthy weight, exercising regularly, and following a balanced diet can help reduce health risks.
What are the treatment options for PCOS? Treatment may include lifestyle changes, medication, or surgery.
Can PCOS be cured? There is no cure for PCOS, but it can be managed effectively.
How often should I see my doctor for PCOS follow-up? Regular follow-up with your doctor is important to monitor your condition and adjust treatment as needed.
Related Articles
Is Obesity Affecting Your Fertility? Link Between Weight and Women's Reproductive Health
Can Weight Loss Fix Your Hormones? Obesity & Hormonal Imbalance
Journal Reference
Silva, G. D. B., Garcia, K. D. T., Ajamyan, H., Shekhawat, P., Rodriguez, L. C., Hammoud, A., De Jesus Avalos Zapata, M., Hernandez, N. F., & Rayon, H. M. R. (2024). Polycystic Ovarian Syndrome: Exploring Hypertension and Cardiometabolic Implications. Cureus. https://doi.org/10.7759/cureus.70958
Image credit: https://www.frontiersin.org/files/Articles/951099/fendo-14-951099-HTML/image_m/fendo-14-951099-g002.
Disclaimer
The information on this website is for informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health care provider with any questions you may have regarding a medical condition or treatment. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
