Obesity and Cardiovascular Disease: Can Antioxidant Balance Reduce Your Risk?
Discover how obesity, oxidative stress, and cardiovascular disease are deeply interconnected. Learn what the latest research reveals about oxidative balance, early BMI risk, and effective prevention strategies to reduce heart disease and mortality.
DR T S DIDWAL MD
4/8/202510 min read
The Complex Relationship Between Obesity, Oxidative Stress, and Cardiovascular Health: What the Latest Research Reveals
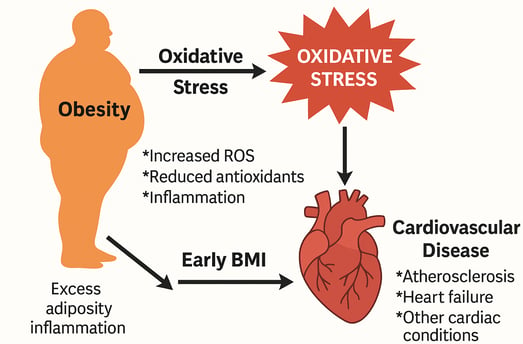
Obesity significantly increases the risk of cardiovascular disease (CVD), with oxidative stress emerging as a key mechanistic link.
Higher Oxidative Balance Scores (OBS), reflecting antioxidant-rich lifestyles, are associated with lower cardiovascular and all-cause mortality in overweight and obese individuals.
Excess weight gain after CVD diagnosis and elevated BMI in early life both independently raise the risk of future cardiovascular events and death.
Targeted interventions—including early prevention, weight stabilization in high-risk patients, and strategies to reduce oxidative stress—are essential to improve long-term cardiovascular outcomes.
The global obesity epidemic has reached alarming proportions, with rates more than doubling over the past four decades. According to the World Health Organization, the percentage of obese adults has increased dramatically from 7% in 1990 to 16% by 2022, with an additional 43% of adults categorized as overweight. This trend represents a significant public health crisis, as excess weight is causally linked to numerous chronic diseases and has been recognized as a disease in itself.
As the global obesity crisis worsens, a growing body of research is uncovering how oxidative stress—an imbalance between harmful reactive oxygen species and protective antioxidants—may be the missing link between obesity and cardiovascular disease (CVD).
New studies reveal that people with higher oxidative balance scores (OBS)—a marker that combines diet, lifestyle, and antioxidant status—have significantly lower mortality risks. In fact, those in the top OBS quartile had a 29.5% reduction in cardiovascular death. This points to oxidative stress not just as a byproduct of obesity but a driving force behind heart damage.
Meanwhile, research shows that weight gain, particularly after a CVD diagnosis, sharply increases mortality risk. Even more concerning, high BMI in youth is tied to heart problems decades later.
The message is clear: managing obesity isn’t just about the scale—it’s about reducing inflammation, reversing oxidative stress, and intervening early. With strategic lifestyle changes, targeted therapies, and sustained public health efforts, we can rewrite the cardiovascular future of millions.
This article examines the latest research on the intricate relationship between obesity, oxidative stress, and cardiovascular outcomes. We'll explore multiple studies that illuminate different aspects of this connection and discuss evidence-based approaches to prevention and management.
Understanding the Obesity-Cardiovascular Disease Connection
Oxidative Balance Score and Mortality Risk in Overweight and Obese Individuals
A groundbreaking study from Hangzhou Third Hospital in China investigated the relationship between oxidative balance and mortality outcomes in overweight and obese individuals. This research utilized data from the National Health and Nutrition Examination Survey (NHANES) from 1999 to 2018, following 26,219 participants with overweight or obesity.
Key findings:
Participants in the highest oxidative balance score (OBS) quartile experienced a 21.7% decrease in all-cause mortality risk and a 29.5% decrease in cardiovascular mortality risk compared to those in the lowest quartile.
The OBS, which combines 15 antioxidants and 5 pro-oxidants derived from lifestyle components and dietary nutrients, provides a comprehensive evaluation of oxidative stress.
Higher OBS scores suggest greater antioxidant capacity and reduced risk of oxidative stress.
White blood cell count and gamma-glutamyl transferase were identified as significant mediators in the association between OBS and mortality risk.
This study highlights how oxidative stress, a common pathophysiological condition in obese individuals, contributes significantly to disease development. The imbalance between antioxidant defenses and reactive oxygen species (ROS) leads to cellular damage, inflammatory responses, and oxidative injuries that elevate disease risk.
Weight Change and Cardiovascular Outcomes in Obese Individuals with Established CVD
A large prospective cohort study using UK Biobank data examined how weight fluctuations affect cardiovascular outcomes, specifically in obese people with established cardiovascular disease. This study followed 8,297 obese participants with CVD over a median duration of 13.9 years.
Key findings:
52.7% of participants maintained relatively stable weight (weight loss or gain <5 kg)
14.2% experienced large weight loss (≥10 kg)
5.1% experienced large weight gain (≥10 kg)
Compared to stable weight, only large weight gain was associated with increased risk of cardiovascular death (HR 3.05) and all-cause mortality (HR 1.93)
This research suggests that among obese individuals with existing cardiovascular disease, preventing significant weight gain may be particularly crucial for reducing mortality risk. The relationship between weight loss and outcomes was more complex, highlighting the need for further research into weight management strategies for this population.
Early-Age BMI and Adulthood Cardiovascular Disease
A comprehensive systematic review and meta-analysis investigated the link between body mass index (BMI) in early age (2-22 years) and cardiovascular diseases in adulthood. This analysis included 38 eligible studies.
Key findings:
BMI in early age was positively associated with:
Overall cardiovascular disease (HR = 1.18)
Coronary heart disease (HR = 1.13)
Heart failure (HR = 1.16)
No significant association was found with stroke (HR = 0.99)
Results remained consistent when stratified by sex, fatal/non-fatal events, and adjustments for socioeconomic status
Both childhood and early adulthood BMI showed positive associations with coronary heart disease and heart failure
Being overweight or obese in youth was associated with adulthood CVDs, including stroke
This meta-analysis underscores the importance of maintaining healthy weight from an early age. The finding that elevated BMI in childhood and early adulthood increases the risk of cardiovascular disease later in life highlights the need for effective obesity prevention and intervention strategies targeting young populations.
European Society of Cardiology: Clinical Consensus on Obesity and Cardiovascular Disease
The European Society of Cardiology has published a comprehensive clinical consensus statement addressing obesity as a major cardiovascular risk factor. This document synthesizes current evidence on multiple aspects of the obesity-cardiovascular disease relationship and provides guidance for implementing evidence-based practices.
Key aspects covered:
Epidemiology and etiology of obesity
Interplay between obesity, cardiovascular risk factors, and cardiac conditions
Clinical management of patients with cardiac disease and obesity
Weight loss strategies including lifestyle changes, interventional procedures, and anti-obesity medications
Impact of weight management on cardiometabolic risk and cardiac outcomes
This consensus statement aims to raise awareness of obesity as a major risk factor and emphasizes the importance of both population-based and personalized approaches to prevent excess weight gain and maintain healthy body weight throughout life.
Practical Implications for Clinicians and Patients
Higher Oxidative Balance Score (OBS) = Lower Mortality:
Patients with higher antioxidant status and healthier lifestyles (as measured by OBS) have significantly lower risk of death from cardiovascular causes.
➡ Clinicians should encourage antioxidant-rich diets and lifestyle habits to improve cardiovascular outcomes.Weight Gain After CVD = Higher Risk:
Obese individuals who gain ≥10 kg after a cardiovascular diagnosis face a 3-fold increased risk of cardiovascular death.
➡ For patients with CVD, the focus should shift from just weight loss to actively preventing further weight gain.Early-Life BMI Predicts Adult Heart Risk:
Elevated BMI between ages 2–22 is linked to higher rates of coronary heart disease and heart failure later in life.
➡ Pediatricians and public health programs must prioritize early obesity prevention as a long-term CVD strategy.Oxidative Stress is a Treatable Target:
Oxidative stress contributes directly to endothelial dysfunction, systemic inflammation, and atherosclerosis in obese individuals.
➡ Addressing oxidative stress through diet, exercise, and possibly pharmacologic means may complement traditional CVD prevention efforts.Stable Weight is Protective—even Without Major Weight Loss:
Among obese patients with CVD, maintaining stable weight showed better survival than significant weight loss or gain.
➡ Individualized care plans should prioritize weight stability when weight loss is not feasible or medically safe.
The Mechanisms Behind Obesity and Cardiovascular Disease
Obesity-Induced Pathophysiological Changes
The relationship between excess adipose tissue and cardiovascular disease involves multiple complex pathways:
Metabolic dysfunction: Adipose tissue in obesity secretes inflammatory cytokines that contribute to insulin resistance, hyperglycemia, and dyslipidemia.
Endothelial dysfunction: Obesity promotes endothelial cell damage, reducing nitric oxide bioavailability and increasing oxidative stress, which initiates atherosclerosis.
Systemic inflammation: Enlarged adipocytes release pro-inflammatory mediators like TNF-α, IL-6, and C-reactive protein, creating a chronic low-grade inflammatory state.
Hemodynamic alterations: Increased blood volume and cardiac output in obesity place additional stress on the heart, contributing to left ventricular hypertrophy and heart failure.
Autonomic nervous system dysfunction: Obesity is associated with increased sympathetic nervous system activity, leading to hypertension and arrhythmias.
Oxidative Stress: A Critical Link
Oxidative stress emerges as a crucial pathway connecting obesity and cardiovascular disease. In obese individuals, several factors contribute to increased oxidative stress:
Elevated ROS production: Excess nutrients lead to mitochondrial dysfunction and increased reactive oxygen species generation.
Reduced antioxidant capacity: Obesity is associated with decreased levels of antioxidant enzymes and vitamins.
Adipose tissue inflammation: Infiltration of immune cells into adipose tissue promotes inflammatory cytokine production and oxidative stress.
Endoplasmic reticulum stress: Excess nutrients trigger ER stress responses that increase ROS production.
The oxidative balance score (OBS) examined in the Hangzhou study provides a valuable tool for assessing this balance between oxidants and antioxidants. The strong inverse association between OBS and mortality outcomes highlights the potential benefits of interventions targeting oxidative balance in obese individuals.
Prevention and Management Strategies
Early Life Interventions
Given the evidence linking early-life BMI with adult cardiovascular disease:
Childhood obesity prevention: School-based programs promoting healthy eating and physical activity are essential components of cardiovascular disease prevention.
Family-based interventions: Engaging parents and caregivers in promoting healthy lifestyle habits from an early age.
Healthcare provider screening: Regular BMI assessment and intervention when necessary during childhood and adolescence.
Comprehensive Weight Management for Adults
For adults with established obesity:
Lifestyle modifications: Structured diet and exercise programs remain the foundation of weight management.
Behavioral interventions: Addressing psychological factors that contribute to weight gain and maintenance.
Pharmacological approaches: Anti-obesity medications that have demonstrated cardiovascular benefits.
Bariatric procedures: Surgical and non-surgical bariatric interventions for appropriate candidates.
Oxidative balance optimization: Dietary patterns rich in antioxidants and lifestyle modifications that reduce oxidative stress.
Special Considerations for Patients with Established CVD
For obese individuals with existing cardiovascular disease:
Preventing further weight gain: Given the clear association between substantial weight gain and increased mortality in this population.
Structured weight loss programs: Supervised by healthcare professionals familiar with cardiovascular disease management.
Cardiac rehabilitation: Incorporating weight management strategies into comprehensive cardiac rehabilitation programs.
Secondary prevention medications: Optimizing cardiovascular medications that may have favorable or unfavorable effects on weight.
FAQ: Obesity and Cardiovascular Disease
Is obesity a risk factor for cardiovascular disease?
Yes, obesity is a major independent risk factor for cardiovascular disease. The research consistently shows that obesity increases the risk of various cardiovascular conditions including coronary artery disease, heart failure, and arrhythmias. According to the European Society of Cardiology, two-thirds of obesity-related excess mortality is attributable to cardiovascular disease.
Does obesity affect survival in systolic heart failure?
The relationship between obesity and heart failure outcomes is complex, sometimes referred to as the "obesity paradox." While obesity increases the risk of developing heart failure, some studies suggest that mildly to moderately obese patients with established heart failure may have better short-term survival than normal-weight patients. However, severe obesity is generally associated with worse outcomes. The mechanisms behind this paradox remain under investigation.
Does weight loss affect long-term cardiovascular disease outcomes?
Weight loss can significantly improve cardiovascular risk factors such as blood pressure, lipid profiles, and glucose metabolism. Studies have shown that intentional weight loss through lifestyle changes, medications, or bariatric surgery can reduce cardiovascular events and mortality. However, the specific amount of weight loss needed for optimal benefits may vary between individuals, and maintaining weight loss long-term is crucial for sustained cardiovascular benefits.
Is early-age BMI a risk factor for cardiovascular disease?
Yes, elevated BMI in childhood and early adulthood is associated with increased cardiovascular disease risk later in life. The meta-analysis discussed in this article found that early-age BMI was positively related to overall cardiovascular disease (HR = 1.18), coronary heart disease (HR = 1.13), and heart failure (HR = 1.16). This underscores the importance of addressing obesity from an early age.
Does abdominal obesity increase risk of all-cause mortality in patients with HFpEF?
Abdominal obesity, characterized by excess visceral fat, is particularly detrimental for cardiovascular health. In patients with heart failure with preserved ejection fraction (HFpEF), abdominal obesity is associated with increased inflammation, more severe symptoms, and worse outcomes including higher all-cause mortality. The distribution of fat (central vs. peripheral) appears to be as important as total fat mass in determining risk.
Can childhood obesity be reversible?
Childhood obesity can be reversed with appropriate interventions, though the difficulty increases with age and duration of obesity. Early intervention programs that include dietary changes, increased physical activity, reduced screen time, and family involvement have shown success in reducing BMI in children and adolescents. However, without sustained healthy behaviors, weight regain is common. The evidence linking childhood obesity with adult cardiovascular disease emphasizes the importance of effective childhood obesity treatment programs.
Call to Action
The mounting evidence linking obesity to cardiovascular disease demands urgent action at multiple levels:
For healthcare providers: Prioritize obesity assessment and management as a key component of cardiovascular disease prevention and treatment. Utilize tools like the oxidative balance score to identify high-risk individuals and monitor intervention effectiveness.
For policymakers: Implement population-level strategies to create environments that support healthy weight maintenance throughout life, with particular attention to children and adolescents.
For individuals: If you're overweight or obese, especially with cardiovascular risk factors or established disease, work with healthcare providers to develop a personalized weight management plan. Focus not only on weight but also on improving dietary quality to enhance oxidative balance.
For researchers: Continue investigating the complex mechanisms linking obesity to cardiovascular disease, particularly the role of oxidative stress, to identify novel intervention targets.
By addressing obesity effectively, we have a tremendous opportunity to reduce the burden of cardiovascular disease worldwide. The research highlighted in this article provides valuable insights to guide these efforts, emphasizing the importance of a lifespan approach to weight management for cardiovascular health.
Related Article
Obesity and Cardiometabolic Risk: Why BMI Isn't Enough | Healthnewstrend
Citations
Koskinas, K. C., Van Craenenbroeck, E. M., Antoniades, C., Blüher, M., Gorter, T. M., Hanssen, H., Marx, N., McDonagh, T. A., Mingrone, G., Rosengren, A., & Prescott, E. B. (2025). Obesity and cardiovascular disease: an ESC clinical consensus statement. European journal of preventive cardiology, 32(3), 184–220. https://doi.org/10.1093/eurjpc/zwae279
Zhang, J., Schutte, R., & Pierscionek, B. (2025). Association of weight change with cardiovascular events and all-cause mortality in obese participants with cardiovascular disease: a prospective cohort study. Heart (British Cardiac Society), heartjnl-2024-324383. Advance online publication. https://doi.org/10.1136/heartjnl-2024-324383
Qiu, Z., Liu, Z., Zhang, N., Fan, F., Weng, H., Zhang, L., Zhang, Y., & Li, J. (2025). Association between early age body mass index and the risk of adulthood cardiovascular diseases: A systematic review and meta-analysis. International Journal of Obesity, 1-10. https://doi.org/10.1038/s41366-024-01710-4
Ying, S., Ding, H., Chen, Y., & Zheng, S. (2025). Association of oxidative balance score with all-cause and cardiovascular mortality in overweight and obese. Frontiers in Nutrition, 12, 1536024. https://doi.org/10.3389/fnut.2025.1536024
Disclaimer
The information on this website is for informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health care provider with any questions you may have regarding a medical condition or treatment. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
About the Author:
Dr.T.S. Didwal, MD, is an experienced Internal Medicine Physician with over 30 years of practice. Specializing in internal medicine, he is dedicated to promoting wellness, preventive health, and fitness as core components of patient care. Dr. Didwal’s approach emphasizes the importance of proactive health management, encouraging patients to adopt healthy lifestyles, focus on fitness, and prioritize preventive measures. His expertise includes early detection and treatment of diseases, with a particular focus on preventing chronic conditions before they develop. Through personalized care, he helps patients understand the importance of regular health screenings, proper nutrition, exercise, and stress management in maintaining overall well-being.
