Obesity and Cardiometabolic Risk: Why BMI Isn't Enough
Discover how obesity and cardiometabolic disease are more complex than BMI alone. Learn about discordant profiles, genetic influences, and precision medicine for better cardiovascular risk assessment and treatment.
DR T S DIDWAL MD
3/30/202513 min read
Obesity and Cardiometabolic Disease: Understanding Discordant Profiles for Precision Medicine
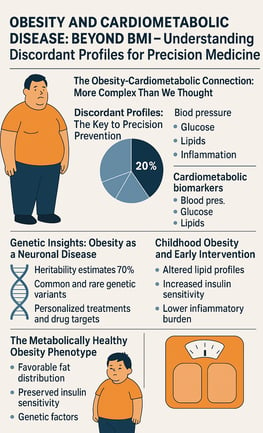
The obesity epidemic and its link to cardiometabolic disease are more complex than once thought. While obesity is a major risk factor for cardiovascular disease, recent research highlights discordant profiles—individuals whose cardiometabolic biomarkers don’t align with their BMI. This means that some people with obesity remain metabolically healthy, while others at normal weight face significant risks.
A groundbreaking European study of 173,000 individuals identified five distinct discordant profiles, affecting 20% of the population. Incorporating these profiles into risk prediction models significantly improved accuracy, potentially preventing unnecessary interventions and ensuring high-risk individuals receive timely care.
Beyond weight alone, genetics plays a crucial role. Obesity is increasingly seen as a neuronal disease, with heritability estimates reaching 70%. While common genetic variants have small effects, rare ones can dramatically increase risk, opening doors to personalized treatments and new drug targets.
The European Society of Cardiology now emphasizes obesity in cardiovascular prevention, urging early intervention, particularly in childhood obesity. Moving forward, integrating biomarker-based assessments into clinical practice could revolutionize prevention strategies. By shifting from a BMI-centered approach to precision medicine, we can better tackle the global burden of cardiometabolic disease.
The Obesity-Cardiometabolic Connection: More Complex Than We Thought
Obesity has more than doubled globally over the past four decades, now affecting over a billion individuals worldwide. Beyond being recognized as a high-risk condition causally linked to numerous chronic illnesses, obesity has been declared a disease in itself—one that significantly impairs quality of life and reduces life expectancy.
A striking statistic emerges from the research: two-thirds of obesity-related excess mortality is attributable to cardiovascular disease. Despite this clear connection, obesity has been historically underrecognized and sub-optimally addressed compared to other modifiable cardiovascular risk factors.
But recent research reveals that the relationship between body mass index (BMI) and cardiometabolic risk is not as straightforward as once believed. Some individuals exhibit what researchers now term "discordant profiles"—where their cardiometabolic biomarkers are either higher or lower than what would be expected based on their BMI alone.
Discordant Profiles: The Key to Precision Prevention
A landmark study conducted across four European population-based cohorts (with approximately 173,000 participants) has shed new light on this phenomenon. Using unsupervised clustering techniques, researchers identified five distinct discordant profiles comprising individuals whose cardiometabolic biomarkers deviated significantly from what would be expected given their BMI.
These discordant profiles collectively represented around 20% of the total population studied—a substantial subgroup whose risk assessment based solely on BMI would be inaccurate. The implications of this finding are profound: one in five individuals may be receiving risk assessments that do not accurately reflect their true cardiometabolic status.
Key Findings from the European Cohort Study
The study revealed that even subtle BMI-discordances in biomarkers significantly affected disease risk. For instance:
A 10% higher probability of having a discordant lipid profile was associated with a 5% higher risk of major adverse cardiovascular events (MACE)
The hazard ratio in women was 1.05 )
The hazard ratio in men was also 1.05
Perhaps most importantly, multivariate prediction models for MACE and type 2 diabetes performed significantly better when they incorporated information about these discordant profiles (likelihood ratio test P < 0.001).
This improvement represents an additional net benefit of 4-15 additional correct interventions and 37-135 additional unnecessary interventions correctly avoided for every 10,000 individuals tested—a meaningful clinical impact at the population level.
The European Society of Cardiology's Position
Recognizing the importance of obesity in cardiovascular health, the European Society of Cardiology has issued a clinical consensus statement that addresses several critical areas:
Current evidence on the epidemiology and etiology of obesity
The interplay between obesity, cardiovascular risk factors, and cardiac conditions
Clinical management strategies for patients with both cardiac disease and obesity
Weight loss strategies including lifestyle modifications, interventional procedures, and anti-obesity medications
The statement places particular emphasis on how these approaches impact cardiometabolic risk and cardiac outcomes. Its primary goals are to raise awareness about obesity as a major risk factor and provide evidence-based guidance for prevention and optimal management within both primary and secondary cardiovascular disease prevention contexts.
Genetic Insights: Obesity as a Neuronal Disease
Adding another layer of complexity to our understanding, recent genetic research has characterized obesity as a heritable neuronal disease with heritability estimates reaching up to 70%. This perspective significantly reshapes how we conceptualize and approach obesity prevention and treatment.
Research reveals that for most individuals, common genetic variants with small effect sizes contribute to obesity risk, which can be further modulated by environmental factors. However, in some cases, rare genetic variants with large effect sizes can influence obesity risk in a Mendelian manner.
The identification of these rare variants has led to several breakthrough insights:
Better understanding of how satiety and reward function as biological processes
Development of more personalized treatment approaches
Identification of potential novel drug targets
These genetic studies have also improved our understanding of the causal mediators between obesity and cardiovascular disease. However, a significant limitation of current genetic research is its focus on populations of European ancestry. Studying more diverse populations will be crucial for developing a more comprehensive understanding of obesity and cardiometabolic disease.
Bridging Research and Clinical Practice
The lessons derived from genetic studies make a compelling case for increasing accessibility to therapies with sustained efficacy in managing obesity and improving overall health. This increased knowledge must also inform public health initiatives aimed at reducing obesity prevalence in coming decades.
The integration of discordant profile information into risk prediction models represents a significant step toward precision medicine in cardiometabolic disease prevention. By looking beyond BMI alone and considering the complex interplay of various biomarkers, clinicians can more accurately identify individuals at highest risk and tailor interventions accordingly.
Childhood Obesity and Early Intervention
Research has also examined the relationship between pediatric obesity and cardiometabolic risk. Altered lipid profiles are frequently associated with childhood obesity, setting the stage for increased cardiometabolic risk later in life. This highlights the importance of early screening and intervention programs targeted at children and adolescents.
Early identification of discordant profiles in younger populations could potentially allow for more effective preventive strategies before cardiometabolic disease develops, potentially altering life-long disease trajectories.
The Role of Ectopic Fat Deposition
Beyond total fat mass, the distribution of adipose tissue significantly influences cardiometabolic risk. Visceral adipose tissue (VAT), which accumulates around internal organs in the abdominal cavity, is metabolically more active and releases more inflammatory mediators than subcutaneous adipose tissue.
Additionally, ectopic fat deposition—the accumulation of triglycerides in non-adipose tissues such as the liver, skeletal muscle, heart, and pancreas—contributes substantially to cardiometabolic risk. For instance:
Hepatic steatosis (fatty liver) is strongly associated with insulin resistance and dyslipidemia
Myocardial steatosis can impair cardiac function and contribute to heart failure
Pancreatic fat may compromise β-cell function and accelerate the development of type 2 diabetes
These mechanisms help explain why some individuals with obesity develop cardiometabolic complications while others do not—differences in fat distribution and ectopic fat deposition may be more important than total fat mass in determining risk.
The Metabolically Healthy Obesity Phenotype
The concept of metabolically healthy obesity (MHO) has emerged to describe individuals with obesity who do not exhibit the metabolic abnormalities typically associated with excess weight. These individuals maintain normal blood pressure, lipid profiles, and glucose homeostasis despite having a BMI ≥30 kg/m².
Research suggests that approximately 10-30% of individuals with obesity may fall into this category, although the prevalence varies depending on the specific criteria used for definition. The MHO phenotype appears to be more common in younger individuals, women, and those with lower BMI within the obesity range.
Several factors may contribute to the MHO phenotype:
Favorable fat distribution: Less visceral and ectopic fat deposition
Preserved insulin sensitivity: Better glucose handling despite excess weight
Lower inflammatory burden: Reduced levels of inflammatory markers
Genetic factors: Certain genetic variants may protect against the metabolic consequences of obesity
However, it's important to note that the stability of the MHO phenotype over time is questionable. Longitudinal studies suggest that many individuals initially classified as MHO eventually develop metabolic abnormalities, particularly with advancing age. This highlights the importance of continued monitoring and preventive measures even in those who appear metabolically healthy.
Normal Weight Metabolic Obesity: The Other Side of the Coin
Conversely, the normal weight metabolic obesity (NWMO) phenotype describes individuals with normal BMI who nonetheless exhibit metabolic abnormalities typically associated with obesity. These individuals have been termed "metabolically obese but normal weight" (MONW).
Characteristics of NWMO include:
Normal BMI (<25 kg/m²)
Insulin resistance
Dyslipidemia (elevated triglycerides, low HDL cholesterol)
Elevated blood pressure
Increased visceral adiposity despite normal total body fat
This phenotype is particularly common in certain Asian populations, where cardiometabolic risk may be elevated at lower BMI thresholds than in populations of European descent. This has led some health authorities to adopt ethnicity-specific BMI cutoffs for overweight and obesity classification.
The NWMO phenotype emphasizes that BMI alone is an imperfect predictor of cardiometabolic risk and that other measures—such as waist circumference, waist-to-hip ratio, or direct assessment of body composition—may provide additional valuable information for risk stratification.
Understanding the Mechanisms: How Obesity Contributes to Cardiometabolic Disease
The pathophysiological mechanisms linking obesity to cardiometabolic disease are multifaceted and complex. Adipose tissue is not merely a passive storage depot; rather, it functions as an active endocrine organ, secreting a variety of bioactive substances collectively known as adipokines. These include:
Leptin: Regulates appetite and energy expenditure
Adiponectin: Exhibits anti-inflammatory and insulin-sensitizing properties
Resistin: Associated with insulin resistance
Inflammatory cytokines: Such as TNF-α and IL-6
In obesity, there is a dysregulation of adipokine production and secretion, with increased levels of pro-inflammatory adipokines and decreased levels of protective ones like adiponectin. This adipokine imbalance contributes to a state of chronic low-grade inflammation, which plays a crucial role in the development of insulin resistance, endothelial dysfunction, and ultimately, cardiometabolic disease.
The Socioeconomic Dimensions of Obesity and Cardiometabolic Disease
Any comprehensive discussion of obesity and cardiometabolic disease must acknowledge the profound influence of socioeconomic factors on both prevention and treatment. These conditions disproportionately affect disadvantaged populations due to:
Food environment: Limited access to affordable, nutritious foods in many low-income areas
Built environment: Lack of safe spaces for physical activity
Healthcare access: Barriers to preventive services and obesity treatment
Work conditions: Long or irregular hours that complicate healthy eating and exercise
Stress: Chronic stress associated with financial insecurity and discrimination
Addressing these social determinants of health is essential for reducing disparities in obesity and cardiometabolic disease burden. Policy interventions that modify the food environment, improve access to healthcare, and address structural inequities have the potential for broad population impact beyond individual-level interventions.
Advances in Treatment: From Lifestyle Interventions to Pharmacotherapy
The management of obesity and associated cardiometabolic risk has evolved significantly in recent years, with an expanding arsenal of evidence-based interventions.
Lifestyle Interventions
Comprehensive lifestyle modification remains the cornerstone of obesity management and includes:
Dietary interventions: Various approaches (e.g., Mediterranean diet, DASH diet, low-carbohydrate diets) have shown efficacy for weight loss and cardiometabolic risk reduction
Physical activity: Regular exercise improves cardiometabolic health even in the absence of significant weight loss
Behavioral therapy: Techniques such as self-monitoring, goal-setting, and problem-solving enhance adherence to lifestyle changes
These interventions are most effective when personalized to individual preferences, cultural background, and specific metabolic abnormalities.
Pharmacotherapy
The field of anti-obesity medications has expanded dramatically in recent years, with several agents demonstrating not only significant weight loss efficacy but also direct cardiometabolic benefits:
GLP-1 receptor agonists (e.g., semaglutide, liraglutide): Originally developed for type 2 diabetes, these medications promote satiety, slow gastric emptying, and reduce food intake. Recent trials have demonstrated significant cardiovascular benefit beyond weight loss alone.
SGLT-2 inhibitors: While not primarily weight loss medications, these agents reduce renal glucose reabsorption and promote modest weight loss while offering substantial cardiorenal protection.
Combination therapies: Emerging approaches combine multiple mechanisms (e.g., GLP-1/GIP dual agonists, GLP-1/glucagon co-agonists) and show promise for enhanced efficacy.
These pharmacotherapeutic advances are particularly important for individuals with discordant profiles, as they may benefit from targeted interventions addressing specific metabolic abnormalities rather than weight loss alone.
Bariatric/Metabolic Surgery
For individuals with severe obesity or those with obesity and established cardiometabolic disease, bariatric surgery (increasingly referred to as metabolic surgery) offers the most effective and durable treatment option. Procedures such as Roux-en-Y gastric bypass and sleeve gastrectomy result in:
Substantial and sustained weight loss
Improvement or resolution of type 2 diabetes, often independent of weight loss
Reduction in cardiovascular events and mortality
Improvement in quality of life
The dramatic metabolic improvements observed after metabolic surgery, often occurring before significant weight loss, have provided valuable insights into the underlying mechanisms linking obesity and cardiometabolic disease.
Personalized Nutrition
The concept of personalized nutrition takes into account individual differences in:
Genetic factors
Microbiome composition
Metabolic responses to different foods
Personal preferences and cultural factors
By tailoring dietary recommendations to individual characteristics, personalized nutrition approaches may enhance both efficacy and adherence compared to one-size-fits-all recommendations.
Key Takeaways
Obesity and cardiometabolic disease often, but not always, coincide – approximately 20% of individuals have "discordant profiles" where their cardiometabolic biomarkers do not align with what would be expected based on their BMI.
Discordant profiles significantly affect disease risk – even subtle BMI-discordances in biomarkers can substantially impact the risk of major adverse cardiovascular events and type 2 diabetes.
Prediction models perform better with discordant profile information – incorporating this information could prevent unnecessary interventions and ensure those at highest risk receive appropriate care.
Obesity has a strong genetic component – characterized as a heritable neuronal disease with heritability estimates up to 70%, involving both common variants with small effects and rare variants with large effects.
Genetic insights have improved understanding and treatment – leading to more personalized approaches and potential new drug targets.
Population diversity in research is needed – most genetic studies to date have focused on European populations, limiting our comprehensive understanding.
Early intervention matters – altered lipid profiles associated with pediatric obesity suggest the importance of early screening and intervention.
A Call to Action
The research findings presented here have significant implications for healthcare providers, policy makers, and individuals:
Consider implementing more comprehensive risk assessment strategies that look beyond BMI alone
Stay informed about emerging research on discordant profiles and their clinical implications
Advocate for more personalized approaches to obesity and cardiometabolic disease prevention
Frequently Asked Questions
Do obesity and cardiometabolic disease always coincide?
No, obesity and cardiometabolic disease often, but not always, coincide. Research has identified "discordant profiles" where individuals have cardiometabolic biomarkers that are higher or lower than would be expected based on their BMI alone. These discordant profiles represent approximately 20% of the population.
Is obesity a risk factor for cardiovascular disease?
Yes, obesity is a major risk factor for cardiovascular disease. In fact, two-thirds of obesity-related excess mortality is attributable to cardiovascular disease. Obesity has been linked to a broad range of cardiovascular disease manifestations including atherosclerotic disease, heart failure, thromboembolic disease, arrhythmias, and sudden cardiac death.
Are altered lipid profiles associated with pediatric obesity and cardiometabolic risk?
Yes, research indicates that altered lipid profiles are frequently associated with pediatric obesity, which can contribute to increased cardiometabolic risk later in life. This highlights the importance of early screening and intervention programs targeted at children and adolescents.
Do subpopulations of cardiometabolic risk differ from BMI?
Yes, research has identified distinct subpopulations where cardiometabolic risk diverges from what would be expected based on BMI alone. These "discordant profiles" can significantly affect disease risk and suggest that precision prevention approaches that look beyond BMI could be more effective.
Do cardiovascular biomarkers increase disease risk independently of BMI?
Yes, cardiovascular biomarkers can increase disease risk independently of BMI. Studies have shown that even subtle BMI-discordances in biomarkers can significantly affect the risk of major adverse cardiovascular events and type 2 diabetes.
Can we predict long-term clinical outcomes attributable to obesity?
Prediction models for obesity-related outcomes like major adverse cardiovascular events and type 2 diabetes perform significantly better when they incorporate information about discordant profiles. This suggests that more comprehensive assessment approaches can improve our ability to predict long-term clinical outcomes attributable to obesity.
Is obesity primarily determined by genetics or environment?
Obesity has a strong genetic component, with heritability estimates reaching up to 70%. However, it is best understood as a complex interaction between genetic predisposition and environmental factors. For most individuals, common genetic variants with small effect sizes contribute to obesity risk, which can be further modulated by environmental factors.
What approaches are most effective for preventing obesity-related cardiovascular disease?
The most effective approaches combine population-based strategies to prevent excess weight gain throughout life with personalized interventions for those with established obesity. The European Society of Cardiology recommends comprehensive weight loss interventions including lifestyle changes, interventional procedures, and anti-obesity medications, with particular focus on their impact on cardiometabolic risk and cardiac outcomes.
Conclusion: A New Paradigm for Prevention
The emerging understanding of the complex relationship between obesity and cardiometabolic disease challenges traditional approaches to risk assessment and intervention. By recognizing and characterizing discordant profiles—subpopulations whose cardiometabolic risk diverges from what would be expected based on BMI alone—we can move toward truly precision-based prevention.
This new paradigm acknowledges that obesity is not a homogeneous condition but rather a complex disease with multiple subtypes, each with distinct risk profiles and treatment needs. By integrating advanced assessment technologies, targeted interventions, and consideration of both genetic and environmental factors, we can improve outcomes for individuals across the BMI spectrum.
The ultimate goal is not simply weight loss, but the prevention of cardiometabolic disease and its complications, thereby improving both quality and quantity of life. The research presented here represents important steps toward this goal, but much work remains to fully implement these insights in routine clinical care.
As we continue to refine our understanding of obesity and cardiometabolic disease, close collaboration between researchers, clinicians, policy makers, and the public will be essential to translate scientific advances into meaningful health improvements for populations worldwide.
Related Articles
How Obesity Triggers Chronic Inflammation: The Immuno-Metabolic Nexus Explained | Healthnewstrend
Should You Be Worried About Homocysteine? What Science Says About Heart Risk | Healthnewstrend
Longevity Secret: Why Cardiorespiratory Fitness, Not Just Fat Loss, Protects Your Heart | Healthnewstrend
https://healthnewstrend.com/obesity-a-growing-problem-but-there-is-hope
https://healthnewstrend.com/keto-diet-and-muscle-friend-or-foe-age-may-hold-the-answer
Obesity Explained: Causes, Health Risks, and Proven Treatments That Work | Healthnewstrend
Citations
Coral, D. E., Smit, F., Farzaneh, A., Gieswinkel, A., Tajes, J. F., Sparsø, T., Delfin, C., Bauvin, P., Wang, K., Temprosa, M., De Cock, D., Blanch, J., Fernández-Real, J. M., Ramos, R., Ikram, M. K., Gomez, M. F., Kavousi, M., Panova-Noeva, M., Wild, P. S., van der Kallen, C., … Franks, P. W. (2025). Subclassification of obesity for precision prediction of cardiometabolic diseases. Nature medicine, 31(2), 534–543. https://doi.org/10.1038/s41591-024-03299-7
Koskinas, K. C., Van Craenenbroeck, E. M., Antoniades, C., Blüher, M., Gorter, T. M., Hanssen, H., Marx, N., McDonagh, T. A., Mingrone, G., Rosengren, A., & Prescott, E. B. (2025). Obesity and cardiovascular disease: an ESC clinical consensus statement. European journal of preventive cardiology, 32(3), 184–220. https://doi.org/10.1093/eurjpc/zwae279
Dash S. (2025). Obesity and Cardiometabolic Disease: Insights From Genetic Studies. The Canadian journal of cardiology, S0828-282X(25)00104-7. Advance online publication. https://doi.org/10.1016/j.cjca.2025.01.034
The Lancet Diabetes Endocrinology (2025). Redefining obesity: advancing care for better lives. The lancet. Diabetes & endocrinology, 13(2), 75. https://doi.org/10.1016/S2213-8587(25)00004-X
Pasarica, M., Dhurandhar, N. V., & Stensel, D. J. (2025). Obesity management with next-generation drugs. International Journal of Obesity, 1-2. https://doi.org/10.1038/s41366-025-01734-4
Disclaimer
The information on this website is for informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health care provider with any questions you may have regarding a medical condition or treatment. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
About the Author:
Dr.T.S. Didwal, MD, is an experienced Internal Medicine Physician with over 30 years of practice. Specializing in internal medicine, he is dedicated to promoting wellness, preventive health, and fitness as core components of patient care. Dr. Didwal’s approach emphasizes the importance of proactive health management, encouraging patients to adopt healthy lifestyles, focus on fitness, and prioritize preventive measures. His expertise includes early detection and treatment of diseases, with a particular focus on preventing chronic conditions before they develop. Through personalized care, he helps patients understand the importance of regular health screenings, proper nutrition, exercise, and stress management in maintaining overall well-being.
