Specialized Pro-Resolving Mediators: A Novel Treatment for Insulin Resistance and Improved Metabolic Health in Obesity
Discover the potential of Specialized Pro-Resolving Mediators (SPMs) in reversing insulin resistance and improving metabolic health. Learn how these powerful compounds can combat obesity and its related complications. Explore the latest research and potential treatment options.
DR T S DIDWAL MD
8/4/20246 min read
According to a review published in Lipids in Health and Disease, obesity is linked to chronic inflammation, leading to insulin resistance and metabolic disorders. Specialized pro-resolving mediators (SPMs), derived from omega-3 and omega-6 fatty acids, actively resolve inflammation, unlike traditional anti-inflammatory drugs. By reducing inflammation, modulating immune cells, and improving insulin sensitivity, SPMs offer a potential breakthrough in treating obesity-related health issues. While research is ongoing, early findings suggest that increasing SPM levels through diet, synthetic analogues, or gene therapy could revolutionize treatment approaches. However, challenges remain in optimizing dosage, delivery, and long-term effects.
Key Points
Obesity and Inflammation: Obesity is linked to chronic low-grade inflammation, which contributes to insulin resistance and metabolic disorders.
SPMs: Nature's Anti-Inflammatories: Specialized Pro-Resolving Mediators (SPMs) are naturally occurring compounds that help resolve inflammation, unlike traditional anti-inflammatory drugs.
How SPMs Work: SPMs act by modulating immune cells, reducing inflammation, and improving insulin sensitivity.
Potential Benefits: SPMs show promise in treating obesity-related conditions like insulin resistance, type 2 diabetes, and fatty liver disease.
Sources of SPMs: Omega-3 fatty acids are precursors to SPMs. Increasing omega-3 intake can boost SPM levels.
Therapeutic Potential: Research is exploring the use of synthetic SPM analogues, gene therapy, and dietary interventions to harness the power of SPMs.
The Power of Specialized Pro-Resolving Mediators in Treating Obesity-Related Insulin Resistance
Obesity has become a global health crisis, affecting millions of people worldwide and leading to serious metabolic complications like insulin resistance and type 2 diabetes. While traditional treatments have shown limited success, an exciting new area of research is emerging around specialized pro-resolving mediators (SPMs)—naturally occurring molecules that could revolutionize how we approach obesity-related metabolic disorders.
In this comprehensive guide, we'll explore the science behind SPMs, their potential benefits for treating obesity and insulin resistance, and what the latest research reveals about these promising compounds. Whether you're struggling with weight issues yourself or are a health professional looking to stay on top of cutting-edge treatments, this article will provide valuable insights into the power of SPMs.
What Are Specialized Pro-Resolving Mediators?
Specialized pro-resolving mediators (SPMs) are a group of bioactive lipid compounds that play a crucial role in resolving inflammation in the body. They are derived from omega-3 and omega-6 polyunsaturated fatty acids and include several families of molecules:
Resolvins
Protectins
Maresins
Lipoxins
Unlike traditional anti-inflammatory drugs that simply suppress inflammation, SPMs actively promote the resolution of inflammation and the return to tissue homeostasis. They act as "stop signals" for inflammatory processes while also stimulating tissue repair and regeneration.
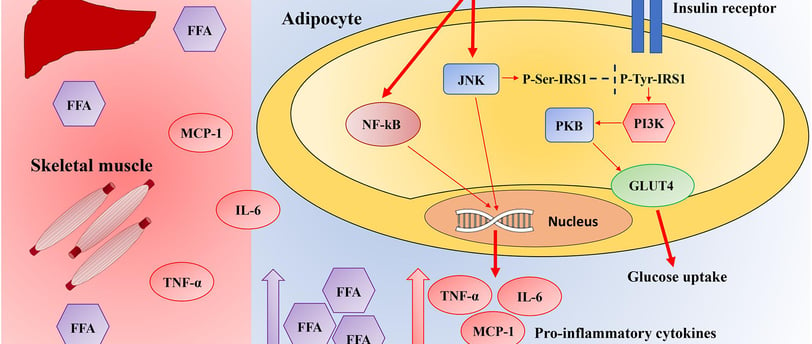
The Connection Between Obesity, Inflammation, and Insulin Resistance
To understand why SPMs are so promising for treating obesity-related metabolic disorders, it's important to recognize the intricate relationship between excess body fat, chronic low-grade inflammation, and insulin resistance:
Adipose tissue dysfunction: As fat cells expand in obesity, they become dysfunctional and attract inflammatory immune cells.
Macrophage infiltration: Increased numbers of pro-inflammatory macrophages infiltrate adipose tissue, creating "crown-like structures" around dying fat cells.
Cytokine production: These activated immune cells release inflammatory cytokines like TNF-α, IL-6, and MCP-1.
Insulin signaling disruption: Chronic inflammation interferes with normal insulin signaling pathways, leading to insulin resistance.
Systemic effects: This localized adipose tissue inflammation spreads systemically, affecting other metabolic tissues like the liver and muscle.
How SPMs Combat Obesity-Related Insulin Resistance
Recent research has uncovered multiple mechanisms by which SPMs can help alleviate insulin resistance and restore metabolic health in obesity:
Modulation of Adipokines and Cytokines
SPMs have been shown to favorably alter the production of key signaling molecules from adipose tissue:
Increase adiponectin: This anti-inflammatory adipokine improves insulin sensitivity.
Decrease leptin: Helps normalize appetite signaling and energy balance.
Reduce pro-inflammatory cytokines: Lowers levels of TNF-α, IL-6, and MCP-1.
Macrophage Phenotype Switching
A hallmark of SPM action is their ability to promote the switching of macrophages from an inflammatory M1 phenotype to an anti-inflammatory M2 phenotype. This helps resolve chronic inflammation in adipose tissue.
Enhanced Phagocytosis
SPMs stimulate macrophages to increase their phagocytic activity, clearing away cellular debris and apoptotic cells more efficiently. This is crucial for resolving inflammation and restoring tissue function.
Regulation of Inflammatory Signaling Pathways
Several key inflammatory signaling cascades are modulated by SPMs:
Activation of AMPK: This master regulator of cellular energy helps improve insulin sensitivity.
Inhibition of NF-κB: A central mediator of inflammatory responses.
Suppression of NLRP3 inflammasome: Reduces the production of pro-inflammatory IL-1β.
Improvement of Insulin Signaling
SPMs have direct effects on insulin signaling pathways:
Increased activation of PI3K/Akt: A critical node in insulin's metabolic actions.
Enhanced GLUT4 translocation: Promotes glucose uptake in muscle and fat cells.
Upregulation of PPARγ: This nuclear receptor is a key regulator of insulin sensitivity.
Alleviation of ER Stress
Endoplasmic reticulum (ER) stress is a significant contributor to insulin resistance in obesity. SPMs have been shown to reduce ER stress through multiple mechanisms, including:
AMPK-mediated autophagy activation
Increased SERCA2b activity
Upregulation of heme oxygenase-1 (HO-1)
Key SPMs in Obesity and Insulin Resistance Research
While there are many types of SPMs, several have shown particular promise in studies of obesity-related metabolic disorders:
Resolvin D1 (RvD1)
Reduces macrophage infiltration in adipose tissue
Promotes M2 macrophage polarization
Improves insulin signaling and glucose uptake
Resolvin E1 (RvE1)
Decreases NLRP3 inflammasome activation
Upregulates GLUT4 and adiponectin expression
Enhances insulin sensitivity
Maresin 1 (MaR1)
Activates AMPK in adipose tissue
Reduces ER stress in liver cells
Improves systemic insulin sensitivity
Protectin DX (PDX)
Alleviates skeletal muscle insulin resistance
Inhibits hepatic gluconeogenesis
Reduces NF-κB activation in adipocytes
Lipoxin A4 (LXA4)
Increases GLUT4 and IRS-1 expression
Enhances insulin-stimulated glucose uptake
Reduces pro-inflammatory cytokine production
Treatmemt Modalities:
1. Lifestyle Modifications
Exercise is crucial: because it improves insulin sensitivity, regulates lipid metabolism, and helps reverse glycemic abnormalities.
2. Medication Options
Metformin: Reduces obesity, improves glucose uptake, and decreases glucose production.
SGLT-2 inhibitors: Increase glucose excretion, lead to weight loss, and improve insulin resistance.
GLP-1 receptor agonists: Reduce appetite, slow stomach emptying, and improve insulin sensitivity.
DPP-4 inhibitors: Maintain blood glucose levels by preventing the breakdown of insulin-stimulating hormones.
3. Anti-Inflammatory Approach
Salicylates: Reduce inflammation, improve insulin sensitivity, and lower blood glucose levels.
4. Challenges and Limitations
Lifestyle changes can be difficult to maintain.
Medications have side effects.
High doses of salicylates can lead to complications.
Conventional anti-inflammatory treatments may weaken the immune system.
5. Need for Further Research
Developing new therapeutic approaches that address inflammation without compromising immune function is essential.
Emerging Therapeutic Approaches Using SPMs
As research on SPMs continues to advance, several promising therapeutic strategies are emerging:
Dietary Supplementation with Omega-3 Fatty Acids
Since SPMs are derived from omega-3 PUFAs like EPA and DHA, increasing dietary intake of these fatty acids may boost endogenous SPM production. Clinical studies have shown benefits of omega-3 supplementation on insulin sensitivity and inflammatory markers in obese individuals.
Development of Synthetic SPM Analogs
Many natural SPMs are chemically unstable, limiting their therapeutic potential. Researchers are working on creating synthetic analogs that maintain biological activity while improving stability and pharmacokinetics.
Gene Therapy Targeting SPM Synthase Enzymes
Enhancing the expression of key enzymes involved in SPM biosynthesis, such as 5-lipoxygenase (5-LOX), may increase endogenous SPM levels and provide metabolic benefits.
Harnessing Brown Adipose Tissue for SPM Production
Recent studies have shown that cold exposure can stimulate brown fat to produce SPM precursors, potentially offering a novel approach to boost SPM levels and improve metabolic health.
Challenges and Future Directions
While the potential of SPMs in treating obesity-related insulin resistance is exciting, several challenges remain:
Optimal dosing and treatment duration: More research is needed to determine the most effective doses and treatment regimens for different SPMs.
Tissue-specific effects: SPMs may have varying effects in different metabolic tissues, requiring careful consideration in therapeutic applications.
Potential side effects: While generally considered safe, long-term effects of SPM supplementation need further study.
Delivery methods: Developing efficient ways to deliver SPMs to target tissues remains a challenge.
Conclusion
Specialized pro-resolving mediators represent a paradigm shift in our approach to treating obesity-related insulin resistance and metabolic disorders. By actively promoting the resolution of chronic inflammation rather than simply suppressing it, SPMs offer a more physiological and potentially safer alternative to traditional anti-inflammatory therapies. The multi-faceted actions of SPMs in modulating adipokine production, macrophage phenotypes, inflammatory signaling pathways, and insulin sensitivity make them uniquely suited to address the complex pathophysiology of obesity-induced insulin resistance. As research in this field continues to advance, we can expect to see the development of novel SPM-based therapies that could revolutionize the treatment of obesity and its metabolic complications.
Journal Reference
Liu, X., Tang, Y., Luo, Y. et al. Role and mechanism of specialized pro-resolving mediators in obesity-associated insulin resistance. Lipids Health Dis 23, 234 (2024). https://doi.org/10.1186/s12944-024-02207-9
Image credit:https://www.frontiersin.org/files/Articles/505887/fphys-10-01607-HTML/image_m/fphys-10-01607-g001.jpg
Related
https://healthnewstrend.com/the-obesity-paradox-how-cardiorespiratory-fitness-combats-heart-disease
https://healthnewstrend.com/how-metabolic-syndrome-and-insulin-resistance-impact-diabetes-treatment
Disclaimer
The information on this website is for informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition or treatment. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
