How Metabolic Syndrome and Insulin Resistance Impact Diabetes Treatment
Metabolic syndrome significantly impacts diabetes management. Understand the connection between these conditions and find out how to optimize treatment outcomes for better health.
DR T S DIDWAL MD
8/4/20249 min read
Metabolic syndrome is highly prevalent among type 2 diabetes patients. This study, published in Frontiers in Clinical Diabetes and Healthcare, found that a staggering 87.5% of participants met the diagnostic criteria, emphasizing its critical role in diabetes management. Key components of the metabolic syndrome, including abdominal obesity, dyslipidemia, and hypertension, were significantly elevated. Despite combined drug therapy, glycemic control remained suboptimal. These findings underscore the urgent need for comprehensive management strategies to address the multifaceted nature of metabolic syndrome and improve outcomes for individuals with type 2 diabetes.
Key Points
High Prevalence of Metabolic Syndrome: The study found an exceptionally high prevalence of metabolic syndrome (87.5%) among type 2 diabetes patients, significantly higher than global averages.
Impact of Age and Gender: The prevalence of metabolic syndrome increased with age and was higher in women than men.
Insulin Resistance and Metabolic Syndrome: All type 2 diabetes patients exhibited insulin resistance, a key factor in developing metabolic syndrome.
Abdominal Obesity: Central obesity was prevalent, especially in women, and linked to insulin resistance, dyslipidemia, and hypertension.
Dyslipidemia: The study identified low HDL levels and high triglyceride levels in most patients, common markers of metabolic syndrome.
Hypertension: A high percentage of patients had elevated blood pressure, another core component of metabolic syndrome.
Poor Treatment Outcomes: Despite combination therapy, most patients had inadequate glycemic control, blood pressure management, and lipid control.
Title: Metabolic Syndrome in Type 2 Diabetes: Prevalence, Impact, and Treatment Challenges
Metabolic syndrome has become a critical global health issue, especially among individuals with type 2 diabetes mellitus (T2DM). A recent study in Yemen highlights the prevalence of metabolic syndrome in T2DM patients and its significant impact on treatment outcomes. This blog post will delve into the key findings of this research and discuss their implications for diabetes management and overall health.
Understanding Metabolic Syndrome
Before discussing the study results, let's briefly review what metabolic syndrome entails. It is a cluster of conditions that occur together, increasing the risk of heart disease, stroke, and type 2 diabetes. According to the National Cholesterol Education Program Adult Treatment Panel III (NCEP ATP III) criteria, metabolic syndrome is diagnosed when an individual has at least three of the following five risk factors:
Abdominal obesity (waist circumference ≥ 88 cm in women and ≥ 102 cm in men)
Elevated blood pressure (≥ 130/85 mmHg) or receiving treatment for hypertension
Fasting blood glucose ≥ 100 mg/dl or receiving treatment for diabetes
Elevated triglycerides ≥150 mg/dl or receiving treatment for elevated triglycerides
Low HDL cholesterol (≤ 50 mg/dl in women and ≤ 40 mg/dl in men) or receiving treatment for low HDL levels
Study Overview
The observational cross-sectional study, conducted between June and December 2023, involved 910 patients with type 2 diabetes mellitus The researchers aimed to investigate the prevalence of metabolic syndrome among T2DM patients and its impact on pharmacotherapy outcomes.
Key Findings
High Prevalence of Metabolic Syndrome
One of the most striking findings of the study was the extremely high prevalence of metabolic syndrome among T2DM patients. A staggering 87.5% of the participants met the criteria for metabolic syndrome. This prevalence is significantly higher than those reported in previous studies from other countries, including the United States (34.2%), India (65%), Egypt (55%), and Ethiopia (53.2%). However, it aligns closely with findings from Saudi Arabia, where 85.8% of T2DM patients were found to have metabolic syndrome.
Age and Gender Differences
The study revealed interesting patterns related to age and gender:
The prevalence of metabolic syndrome increased with age, ranging from 71.2% in patients under 35 years old to 96.3% in those over 75 years old.
Metabolic syndrome was more prevalent among female patients (91.3%) compared to male patients (83.9%).
Distribution of Risk Factors
The researchers examined the distribution of metabolic syndrome risk factors among the participants:
Insulin resistance: 100% (as all participants had T2DM)
Low HDL cholesterol: 95.3%
Elevated blood pressure: 83%
Triglyceride dyslipidemia: 80.1%
Abdominal obesity: 62.5%
Notably, abdominal obesity was far more prevalent among female patients (84%) compared to male patients (42.6%).
Impact on Treatment Outcomes
The study revealed concerning data regarding the management of T2DM and its associated comorbidities:
Only 12% of patients achieved adequate glycemic control.
Among patients with hypertension, only 40.9% achieved proper blood pressure control.
For those with dyslipidemia, just 29% attained adequate management.
Metabolic Syndrome and Treatment Efficacy
The presence of metabolic syndrome appeared to negatively impact treatment outcomes:
Blood pressure control was achieved in 34.4% of patients with metabolic syndrome, compared to 77.2% in those without.
Dyslipidemia was controlled in 26.9% of patients with metabolic syndrome, versus 47.3% in those without.
Treatment Patterns
The study also provided insights into the pharmacological management of T2DM:
64.3% of patients received combination therapy
34.4% were on monotherapy
5.3% were prescribed triple therapy
The most common treatment regimen was a combination of metformin and sulfonylureas, prescribed to 58.6% of patients.
Implications and Discussion
The high prevalence of metabolic syndrome among T2DM patients in this study is alarming and highlights the need for comprehensive approaches to diabetes management. Several factors may contribute to this high prevalence, including:
Lifestyle Factors: The modern sedentary lifestyle, combined with poor dietary habits, likely plays a significant role in the development of metabolic syndrome.
Genetic Predisposition: There may be genetic factors that make certain populations more susceptible to metabolic syndrome.
Late Diagnosis: The high prevalence could indicate that metabolic syndrome is often diagnosed late, after multiple risk factors have already developed.
Lack of Preventive Interventions: There may be insufficient focus on preventive measures and early interventions to address the components of metabolic syndrome.
The gender disparity in abdominal obesity (84% in women vs. 42.6% in men) is particularly noteworthy. This could be attributed to cultural factors in Yemen, where women may have fewer opportunities for physical activity and may adhere to more sedentary lifestyles. The poor treatment outcomes observed in this study are concerning. Only a small percentage of patients achieved adequate control of blood glucose, blood pressure, and lipid levels. This suggests that current treatment approaches may be insufficient or that patient adherence to prescribed therapies is suboptimal.
The negative impact of metabolic syndrome on treatment efficacy for hypertension and dyslipidemia underscores the importance of addressing metabolic syndrome as a whole, rather than treating its components in isolation.
Recommendations
Based on the study findings, several recommendations can be made:
Early Screening and Intervention: Healthcare providers should implement regular screening for metabolic syndrome, particularly in individuals at high risk for T2DM. Early detection can lead to timely interventions that may prevent or delay the onset of T2DM and its complications.
Comprehensive Management Approach: Treatment strategies should address all components of the metabolic syndrome simultaneously. This may involve a combination of lifestyle modifications and pharmacological interventions.
Personalized Treatment Plans: Given the high prevalence of metabolic syndrome and the variability in risk factors, treatment plans should be tailored to each patient's specific needs and risk profile.
Patient Education: Improved patient education about metabolic syndrome, its consequences, and the importance of adherence to treatment plans is crucial for better outcomes.
Focus on Lifestyle Modifications: Encourage and support patients in making sustainable lifestyle changes, including adopting a healthy diet, increasing physical activity, and maintaining a healthy weight.
Regular Monitoring: Implement more frequent monitoring of blood glucose, blood pressure, and lipid levels to allow for timely adjustments to treatment plans.
Address cultural and gender-specific factors: Develop strategies to promote physical activity and healthy lifestyles that are culturally appropriate, particularly for women in conservative societies.
Investigate New Biomarkers: Further research into new biomarkers, such as the NLRP3 inflammasome and its downstream cytokines, may provide new insights into the pathogenesis of metabolic syndrome and lead to novel therapeutic approaches.
Limitations and Future Research
While this study provides valuable insights, it has some limitations. As an observational cross-sectional study, it cannot establish causal relationships. Future research should focus on:
Longitudinal Studies: Conduct long-term studies to better understand the progression of metabolic syndrome and its impact on T2DM outcomes over time.
Intervention Studies: Design and implement studies that evaluate the effectiveness of various interventions in preventing and managing metabolic syndrome in T2DM patients.
Genetic and Environmental Factors: Investigate the interplay between genetic predisposition and environmental factors in the development of metabolic syndrome.
Conclusion
This study highlights the alarmingly high prevalence of metabolic syndrome among patients with type 2 diabetes mellitus and its significant impact on treatment outcomes. The findings underscore the need for a paradigm shift in how we approach diabetes management, moving towards more comprehensive, personalized, and proactive strategies that address all components of metabolic syndrome. By focusing on early detection, comprehensive management, and patient-centred care, healthcare providers can work towards improving outcomes for T2DM patients and reducing the burden of associated cardiovascular complications. Moreover, addressing the broader societal and cultural factors that contribute to the development of metabolic syndrome is crucial for long-term success in combating this growing health challenge. As we continue to unravel the complex interplay between metabolic syndrome and type 2 diabetes, it is clear that a multifaceted approach involving healthcare providers, policymakers, and patients themselves will be necessary to turn the tide on this global health issue.
1. What is metabolic syndrome, and how is it related to type 2 diabetes?
Metabolic syndrome is a cluster of conditions that increase the risk of heart disease, stroke, and type 2 diabetes. It includes abdominal obesity, elevated blood pressure, high blood sugar levels, high triglycerides, and low HDL cholesterol. In individuals with type 2 diabetes, metabolic syndrome is particularly common and can exacerbate the complications and management challenges of diabetes.
2. Why is metabolic syndrome more prevalent among people with type 2 diabetes?
People with type 2 diabetes are more likely to have metabolic syndrome due to common underlying factors such as insulin resistance and obesity. These factors contribute to the development of both conditions. Additionally, the presence of diabetes can worsen the other components of the metabolic syndrome, creating a cycle that increases prevalence.
3. What are the risk factors for developing metabolic syndrome?
The risk factors for metabolic syndrome include abdominal obesity, elevated blood pressure, high fasting blood glucose, elevated triglycerides, and low HDL cholesterol. Lifestyle factors such as poor diet, lack of physical activity, and genetic predisposition also play significant roles in its development.
4. How does metabolic syndrome affect treatment outcomes in type 2 diabetes?
Metabolic syndrome can negatively impact treatment outcomes in type 2 diabetes by making it more difficult to control blood glucose, blood pressure, and lipid levels. The presence of multiple risk factors often necessitates more complex and aggressive treatment plans, and even then, achieving adequate control can be challenging.
5. What lifestyle changes can help manage metabolic syndrome in people with type 2 diabetes?
Managing metabolic syndrome in people with type 2 diabetes involves lifestyle changes such as adopting a healthy diet rich in fruits, vegetables, and whole grains, increasing physical activity, maintaining a healthy weight, quitting smoking, and reducing alcohol intake. These changes can help improve all components of the metabolic syndrome.
6. Why is metabolic syndrome more prevalent in women compared to men?
In the context of the study from Yemen, metabolic syndrome was more prevalent in women, possibly due to cultural and societal factors that limit physical activity and promote sedentary lifestyles. Additionally, women may have higher rates of abdominal obesity, which is a key component of metabolic syndrome.
7. What are the treatment options for metabolic syndrome in type 2 diabetes patients?
Treatment options for metabolic syndrome in type 2 diabetes patients include lifestyle modifications (diet and exercise), pharmacological interventions to manage blood glucose, blood pressure, and cholesterol levels, and possibly weight-loss surgery in severe cases. Medications commonly used include metformin, sulfonylureas, antihypertensives, and lipid-lowering drugs.
8. How does early detection of metabolic syndrome benefit individuals with type 2 diabetes?
Early detection of metabolic syndrome allows for timely intervention, which can prevent or delay the onset of complications associated with type 2 diabetes. By identifying and managing risk factors early, healthcare providers can implement strategies to improve overall health outcomes and reduce the burden of cardiovascular and metabolic diseases.
9. What role do genetic factors play in the development of metabolic syndrome?
Genetic factors can contribute to an individual's susceptibility to metabolic syndrome by influencing how the body stores fat, processes glucose, and regulates blood pressure and cholesterol levels. Understanding these genetic predispositions can help tailor prevention and treatment strategies for those at higher risk.
10. How can healthcare providers address cultural and gender-specific factors in managing metabolic syndrome?
Healthcare providers can address cultural and gender-specific factors by developing culturally appropriate health education programs, promoting physical activity through community-based initiatives, and providing gender-sensitive support and resources. Engaging with community leaders and understanding local practices can enhance the effectiveness of these interventions.
Journal Reference
Alawdi, S. H., & Alshawky, S. (2024). Metabolic Syndrome in Patients with Type 2 Diabetes Mellitus and its Impact on Pharmacotherapy Outcomes. Frontiers in Clinical Diabetes and Healthcare, 5, 1380244. https://doi.org/10.3389/fcdhc.2024.1380244
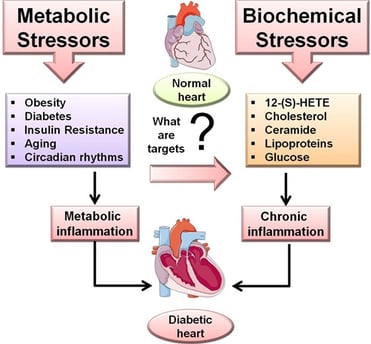
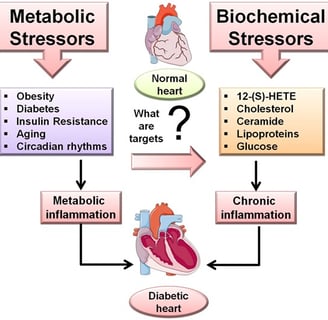
Image credit:https://www.frontiersin.org/files/Articles/258167/fcvm-04-00031-HTML/image_m/fcvm-04-00031-g001.jpg
Related
https://healthnewstrend.com/shift-work-sleep-loss-and-diabetes-is-your-circadian-clock-at-risk
Disclaimer
The information on this website is for informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition or treatment. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
